|
Tadapox dosages: 80 mg
Tadapox packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills

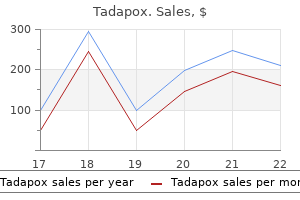
Discount tadapox 80mg without a prescriptionEach artery divides into branches that accompany the segmental and subsegmental bronchi erectile dysfunction in teens buy cheap tadapox 80mg online, mostly in a posterolateral position impotence nhs order discount tadapox. The pulmonary capillaries form single-layered and exceedingly thin-walled plexuses immediately exterior the epithelium in the walls and septa of the alveoli and alveolar sacs erectile dysfunction book buy cheap tadapox 80mg on line. Pulmonary veins erectile dysfunction at age 18 buy tadapox 80 mg overnight delivery, two from each lung, drain the pulmonary capillaries; their rootlets coalesce into bigger and more freely speaking veins that traverse the lung, for the most half independently of the pulmonary arteries and bronchi. At the hilum, the pulmonary vessels accompany the primary bronchial divisions; the veins are anteromedial and the arteries posterolateral to the bronchi. Some veins also lie beneath the visceral pleura, including the pleura within the interlobar fissures. This sample of bronchi, arteries and veins displays considerable variation; veins are essentially the most variable, and arteries are more variable than bronchi. Extralobar pulmonary sequestration segments are covered by visceral pleura and usually discovered under the left inferior lobe, whereas intralobar abnormalities are often embedded in regular lung: classically, the posterior basal segment of the left inferior lobe. Extralobar pulmonary 959 chaPter 54 Pleura, lungs, trachea and bronchi Unilateral absence of a pulmonary artery is a rare congenital abnormality characterised by normal lung volume and anatomy at delivery. Revascularization before the age of 6 months avoids the event of lung hypoplasia (Alison et al 2011). The left pulmonary artery sling is a congenital abnormality characterised by the left pulmonary artery arising from the best pulmonary artery, coursing over the right principal bronchus and heading posteriorly between the trachea and oesophagus. This abnormality is related to vital tracheobronchial stenosis (Zhong et al 2010). Consideration of differential analysis with mediastinal or pulmonary tumours is mandatory. They originate from capillary networks within the alveolar partitions and return oxygenated blood to the left atrium. All the main tributaries of the pulmonary veins obtain smaller tributaries, each intra- and intersegmental; by serial 960 junctions, tributary veins lastly kind a single lobar trunk, i. The proper middle and superior lobar veins often unite and so two veins, superior and inferior, leave each lung. The superior pulmonary vein is anteroinferior to the pulmonary artery, and the inferior pulmonary vein is probably the most inferior hilar construction and in addition slightly posterior. On the proper, the union of apical, anterior and posterior veins (draining the higher lobe) with a middle lobar vein formed by lateral and medial tributaries constitutes the right superior pulmonary vein. The proper inferior pulmonary vein is shaped by the hilar union of superior (apical) and common basal veins from the decrease lobe. The right superior pulmonary vein passes posterior to the superior vena cava, the inferior behind the proper atrium. The superior left pulmonary vein is formed by the union of apicoposterior, anterior and lingular veins. The left inferior pulmonary vein is formed from the union of the superior (apical) and common basal Pleura, lungs, trachea and bronchi A thrombus that has developed within the deep veins (usually leg or pelvic) could embolize and travel in the best side of the circulation via the best atrium and ventricle, lodging within the pulmonary vasculature. The clinical abnormalities observed depend upon the size of the embolus and on the number and frequency of embolic episodes. Large emboli may lodge in the primary pulmonary artery branches and trigger proper ventricular dysfunction and hypoxia, representing a medical emergency. Pulmonary emboli trigger a ventilation/perfusion mismatch that may have critical physiological implications resulting in a major discount within the oxygenation of blood. Ventilation/perfusion scans with radiolabelled xenon and technetium normally show segmental abnormalities in perfusion with regular ventilation within the corresponding regions. Repetitive embolization may eventually lead to a dramatic reduction of the pulmonary vascular bed and chronic cor pulmonale. Thrombolysis, anticoagulation or inferior vena caval filters stop development or recurrence of embolism. A clot may traverse a patent foramen ovale and lodge within the arterial system (paradoxical embolism), most severely within the cerebral circulation, inflicting a stroke (Kent and Thaler 2011). Both left superior and inferior pulmonary veins move anterior to the descending thoracic aorta. Sometimes, the two left pulmonary veins type a single trunk, or they might be augmented by an accessory lobar vein from every lobe, which unite to kind a 3rd left pulmonary vein. Their terminations are separated medially by the indirect pericardial sinus, and laterally by smaller and variable pulmonary venous pericardial recesses which are directed superomedially. The variable incorporation of the primitive pulmonary vein into the left atrium implies that the number of main pulmonary veins might differ. The left atrium is the heart chamber most posterior and median in place, and so the length of the left and proper pulmonary veins is equal, in distinction to the arteries and bronchi, the place there are conspicuous left�right differences in size. The terminal elements of the pulmonary veins are surrounded by atrial myocardium; these areas characterize potential accent re-entrant circuits answerable for the initiation or maintenance of supraventricular tachycardias or atrial fibrillation and could also be percutaneously ablated. The anterior plexus is small and is formed by rami from vagal and sympathetic cervical cardiac nerves via connections with the superficial cardiac plexus. The posterior pulmonary plexus is formed by the rami of vagal and sympathetic cardiac branches from the second to fifth or sixth thoracic sympathetic ganglia. Further details of the pulmonary plexuses are given in the description of the cardiac plexuses on web page 1021. The sympathetic nervous system (noradrenaline (norepinephrine)) appearing on -receptors produces bronchodilation; the parasympathetic nervous system (acetylcholine) performing on muscarinic M3 receptors maintains Lymphatic drainage the pulmonary lymphatics originate in superficial and deep plexuses. The superficial plexus lies deep to the visceral pleura; its efferents flip around the margins of the lung and its fissures, eventually reaching the bronchopulmonary nodes. The deep lymphatics originate at bronchiolar level and follow the bronchovascular divisions to the hilum, ending in the same nodes. No free anastomoses exist between the two methods, besides at the hilum and peripherally, where small but dilatable channels connect superficial and 961 chaPter deep lymphatic vessels; these connections direct lymph from the deep to the superficial channels when outflow from deep vessels is obstructed by pulmonary disease. There is a bent for vessels from the superior lobes to move to the superior tracheobronchial nodes, and those from the inferior lobes to move to the inferior tracheobronchial group. At the level of pulmonary lobation, the association of lymphatic vessels follows the central artery of a lobule and its peripheral veins. The numbers in the lower figure denote the numbers of the bronchopulmonary segments. Their partitions comprise two types of epithelial cell (pneumocytes) and canopy a delicate connective tissue within which a community of capillaries ramifies. Since the partitions are extraordinarily thin, they present a minimal barrier to gaseous change between the atmosphere and the blood within the capillaries. Adjacent alveoli are incessantly in close contact; the intervening connective tissue varieties the central a part of the interalveolar septum. Alveolar macrophages are current throughout the alveolar lumen and migrate over the epithelial floor. The alveolar lining epithelium varies in thickness, but in depth areas of it are as little as zero. The whole barrier to diffusion between air and blood in these thin parts could additionally be as little as 0. Alveolar space Both human lungs comprise 300�500 million alveoli, giving a total surface space of 70�100 m2. These values range significantly between normal younger people; the variations turn into even more marked with age and as a consequence of degenerative changes. The number of alveoli will increase from approximately 10 million at delivery to the grownup value, primarily in the first eight years; thereafter, the rise in lung volume is achieved through augmentation of alveolar volume (Narayanan et al 2013). Their inflated diameter varies with lung position, and is greater within the superior regions than in the inferior because of the elevated gravitational strain at the lung base. Although the lung enlarges in all instructions during inspiration, many of the change in quantity seems to be as a result of the lengthening and growth of the alveolar ducts and increase in the measurement of the openings into the air sacs; the inspiratory change in the volume of the gas-conducting system is insignificant. Type I pneumocytes are easy squamous epithelial cells and type over 90% of the alveolar space. Blue is used for vessels that comprise deoxygenated blood, and red for vessels that include oxygenated blood. Together with an identical endothelial barrier, this association limits the motion of fluid from blood and interstitial areas into the alveolar lumen (the blood�air barrier).
Cheap 80 mg tadapox visaKey: 1 erectile dysfunction enlarged prostate buy tadapox cheap, anterior junction; 2 erectile dysfunction after age 50 cheap tadapox 80mg with mastercard, superior vena cava; 3 impotence in a sentence cheap 80mg tadapox amex, pretracheal space; four erectile dysfunction pills review generic 80mg tadapox mastercard, trachea; 5, arch of aorta; 6, oesophagus; 7, scapula. Key: 1, ascending aorta; 2, superior vena cava; 3, right pulmonary artery; 4, right principal bronchus; 5, subcarinal space; 6, oesophagus; 7, azygos vein; 8, trunk of pulmonary artery; 9, left superior pulmonary vein; 10, left principal bronchus; eleven, inferior department of the left pulmonary artery; 12, descending aorta. Key: 1, aortic root; 2, left atrium; 3, oesophagus; four, azygos vein; 5, right ventricular outflow tract; 6, left inferior pulmonary vein; 7, descending aorta. A, Key: 1, right brachiocephalic vein; 2, left brachiocephalic vein; 3, pulmonary trunk; 4, ascending aorta; 5, left ventricle; 6, proper atrium. C, Key: 1, brachiocephalic trunk; 2, left frequent carotid artery; 3, aortic arch; four, superior vena cava; 5, pulmonary trunk; 6, left ventricle; 7, abdominal aorta. D, Key: 1, proper subclavian artery; 2, trachea; 3, aortic arch; 4, left major pulmonary artery; 5, right primary pulmonary artery; 6, left superior pulmonary vein; 7, left atrium; 8, descending thoracic aorta. E, Key: 1, left subclavian artery; 2, trachea; 3, posterior aortic arch; four, left primary pulmonary artery; 5, left atrium; 6, descending thoracic aorta. Key references pretracheal, subcarinal, proper paratracheal, posterior tracheal and aortopulmonary window stations are frequent websites of lymph node metastases in lung cancer. The aortopulmonary window is located between the aortic arch superiorly and the left pulmonary artery inferiorly; the trachea varieties its medial border and the left lung its lateral border. The proper paratracheal house lies between the best lung and the trachea on its anterolateral facet; the posterior tracheal space between the lung and the posterolateral side of the trachea; and the subcarinal area inferior to the carina bounded by the principal bronchi. On the proper, the azygo-oesophageal recess is situated posterior to the subcarinal space and on the left facet is the oesophagus. All these areas are in direct continuity with each other and are inspected during transcervical mediastinoscopy. The anterior junction lies between the great vessels, posterior margin of the chest wall and the lungs where the left brachiocephalic vein, highest mediastinal nodes, thymus and phrenic nerves are positioned. The posterior junction is an area posterior to the trachea and is the place the lungs appose. The paraspinal area lies between the lateral margins of the backbone and the lungs the place the intercostal vessels, the ganglionated sympathetic chain and small lymph nodes are located. The retrocrural space, between the diaphragmatic crura and vertebral our bodies, is traversed by the aorta, azygos venous system, thoracic duct, intercostal arteries, sympathetic chains and splanchnic nerves. Surgical administration includes pleurectomy, talc poudrage, pleuroperitoneal shunting or repair/ligation of the thoracic duct. An clarification of how damage or disease of the thoracic duct or its main tributaries can lead to a chylous effusion, identified by fluid assaying for triglyceride content and lipid electrophoreses for chylomicrons. Conservative administration choices embrace remark, treatment of the underlying disease, strict medium-chain triglyceride diet or whole parenteral vitamin, thoracocentesis, tube thoracostomy with chemical pleurodesis or thoracic duct embolization. Gofeld M, Faclier G 2006 Bilateral ache relief after unilateral thoracic percutaneous sympathectomy. Kawashima T 2011 Anatomy of the cardiac nervous system with scientific and comparative morphological implications. Morphological studies are described from macroscopic, scientific and evolutionary anatomical viewpoints, together with their functions in enhancing surgical technique and for future evaluation in regenerative drugs. Kuntz A 1927 Distribution of the sympathetic rami to the brachial plexus: its relation to sympathectomy affecting the upper extremity. A description of the numerous variety of individuals in whom the intrathoracic somatic branches from the second thoracic spinal nerve join the first thoracic spinal nerve. Raica M, Encic S, Motoc A et al 2006 Structural heterogeneity and immunohistochemical profile of Hassall corpuscles in regular human thymus. Segni M, di Nardo R, Pucarelli I et al 2011 Ectopic intrathyroidal thymus in youngsters: a long-term follow-up research. Varga I, Uhrinova A, Toth F et al 2011 Assessment of the thymic morphometry utilizing ultrasound in full-term newborns. An exploration of how the artery of Adamkiewicz should be recognized in patients with thoracoabdominal aortic aneurysm to help surgical planning and to keep away from postoperative paraplegia. It is troublesome and very harmful to consider with selective intercostal or lumbar angiography. The fibrous pericardium is a sac manufactured from robust connective tissue, fully surrounding and unattached to the center. It develops through a sequential means of cavitation of the embryonic body wall by expansion of the secondary pleural cavity; its lateral walls are thus clothed by parietal mediastinal pleura. The serous pericardium consists of two layers, one inside the opposite; the internal (visceral) serosal layer adheres to the heart and varieties its outer covering, often recognized as the epicardium, whereas the outer (parietal) serosal layer adheres to the interior surface of the fibrous pericardium. These two serosal surfaces are apposed and separated by a movie of fluid, which permits unbiased movement of the internal membrane and its adherent coronary heart, constituting two parietovisceral traces of serosal reflection. The separation of the two membranes of the serous pericardium creates a narrow pericardial cavity that provides complete cleavage between the heart and its environment, allowing freedom of cardiac movement and shape change. Anteriorly, the fibrous pericardium is separated from the thoracic wall by the lungs and pleural coverings. However, in a small space behind the decrease left half of the body of the sternum and the sternal ends of left fourth and fifth costal cartilages, the pericardium is in direct contact with the thoracic wall. Until it regresses, the decrease finish of the thymus can be anterior to the upper pericardium. The principal bronchi, oesophagus, descending thoracic aorta and posterior elements of the mediastinal floor of both lungs are all posterior relations. The phrenic neurovascular bundle descends bilaterally between the fibrous pericardium and mediastinal pleura. In this image with a section thickness of 10 mm, the pericardium seems as a skinny, curvilinear construction (arrows). The pericardium is often greatest visualized alongside the best facet of the center due to surrounding fats. With growing part thickness, maximal pericardial thickness (measured alongside the proper ventricle) will increase from zero. The aorta, superior vena cava and the pulmonary arteries and veins all receive extensions of the fibrous pericardium but the inferior vena cava traversing the central tendon has no such overlaying. The perivenous tube is an inverted J; the cul-de-sac inside its curve posterior to the left atrium is termed the indirect sinus. Serous pericardium the serous pericardium is a closed sac inside the fibrous pericardium and has visceral and parietal layers. The visceral layer, or epicardium, covers the guts and great vessels, and is reflected into the parietal layer, which lines the inner floor of the fibrous pericardium. The visceral layer of the serous pericardium is a single layer composed of ciliated mesothelial cells on a skinny subserosal layer of connective tissue ample in elastic fibres, blending with the fibrous pericardium at the parietal membrane and with the interstitial myocardial tissue at the visceral membrane. The serosal cilia enhance the surface area for fluid production and resorption, along with reducing friction between the opposing pericardial layers. The cardiac subserosal layer incorporates fat, particularly alongside the ventricular facet of the atrioventricular and interventricular grooves and the inferior cardiac border. The major coronary vessels and their bigger branches are embedded in this fats; the quantity is said to the general extent of physique fats and steadily increases with age. The amount of epicardial adipose tissue could additionally be a cardiometabolic threat issue, with growing thickness linked to metabolic syndrome and diabetes mellitus. A vital correlation has been demonstrated Pericardial area and fluid the pericardial cavity is the house fashioned between the parietal and visceral layers of the serous pericardium. The pericardial cavity covers the proximal a part of the nice vessels and the vast majority of the center, extending between the left atrium and the descending thoracic aorta; the left pleural area extends posterior to the descending aorta. The pericardial cavity normally contains roughly 15�20 ml of serous plasma ultrafiltrate. Refer to the textual content for extra named recesses of the overall serous pericardial cavity and its transverse sinus. From the principal pericardial cavity, the postcaval recess tasks towards the left, behind the atrial termination of the superior vena cava, restricted superiorly by the right pulmonary artery and inferiorly by the superior right pulmonary vein, with its mouth opening superolaterally to the best. The right and left pulmonary venous recesses every project superomedially on the posterior floor of the left atrium between the superior and inferior pulmonary veins on both sides, indenting the side walls of the indirect sinus. The superior aortic recess extends from the transverse sinus; through its inferior mouth, it ascends posterior to , then to the right of, the ascending aorta and ends on the stage of the sternal angle.
Buy line tadapoxThey are usually found as a pair of our bodies lying anterolateral to the aorta in the area of the inferior mesenteric and superior hypogastric plexuses erectile dysfunction and urologist buy generic tadapox 80mg line, but multiple smaller collections may be current erectile dysfunction diet order tadapox 80 mg overnight delivery. Scattered cells that persist into adulthood may erectile dysfunction lack of desire cheap tadapox master card, rarely erectile dysfunction pills over the counter buy 80mg tadapox with visa, be the sites of paraganglioma (extra-adrenal phaeochromocytoma) (Subramanian and Maker 2006). Together with Klaassen et al 2011, these two papers provide a useful description of the anatomy of the ilioinguinal and iliohypogastric nerves and underline the significance of the ilioinguinal nerve in clinical apply. This article revises conventional ideas in regards to the cisterna chyli and its formation. Biglioli P, Roberto M, Cannata A et al 2004 Upper and decrease spinal cord blood supply: the continuity of the anterior spinal artery and the relevance of the lumbar arteries. Coffin A, Boulay-Coletta I, Sebbag-Sfez D et al 2015 Radioanatomy of the retroperitoneal area. Making sense of mesocolic anatomy based on findings from fashionable investigative strategies. Culligan K, Walsh S, Dunne C et al 2014 the mesocolon: a histological and electron microscopic characterization of the mesenteric attachment of the colon previous to and after surgical mobilization. Hebbard P, Ivanusic J, Sha S 2011 Ultrasound-guided supra-inguinal fascia iliaca block: a cadaveric analysis of a novel approach. Katritsis E, Anagnostopoulou S, Papadopoulos N 1980 Anatomical observations on the accent obturator nerve (based on a thousand specimens). Kimura W, Yano M, Sugawara S et al 2010 Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein: techniques and its significance. Kirchmair L, Lirk P, Colvin J et al 2008 Lumbar plexus and psoas main muscle: not all the time as anticipated. Together with Ndiaye et al 2007, these two papers provide a useful description of the anatomy of the ilioinguinal and iliohypogastric nerves and underline the importance of the ilioinguinal nerve in medical apply. Lolis E, Panagouli E, Venieratos D 2011 Study of the ascending lumbar and iliolumbar veins: surgical anatomy, scientific implications and evaluation of the literature. Loukas M, Hullett J, Wagner T 2005a Clinical anatomy of the inferior phrenic artery. Loukas M, Pinyard J, Vaid S et al 2007a Clinical anatomy of celiac artery compression syndrome: a review. Moro T, Kikuchi S, Konno S et al 2003 An anatomic study of the lumbar plexus with respect to retroperitoneal endoscopic surgery. Pa�o B, Sebasti� C, Bu�esch L et al 2011 Pathways of lymphatic unfold in male urogenital pelvic malignancies. Phang K, Bowman M, Phillips A et al 2014 Review of thoracic duct anatomical variations and clinical implications. Phillips S, Mercer S, Bogduk N 2008 Anatomy and biomechanics of quadratus lumborum. Spentzouris G, Zandian A, Cesmebasi A et al 2014 the clinical anatomy of the inferior vena cava: a evaluation of common congenital anomalies and issues for clinicians. Toni R, Mosca S, Favero L et al 1988 Clinical anatomy of the suprarenal arteries: a quantitative strategy by aortography. An evidence-based evaluate of the advanced and clinically essential thoracolumbar fascia. Passage across the midline to the left subphrenic area is prevented by the falciform ligament. Malignant cells might turn into trapped within peritoneal recesses or in the milky spots of the larger omentum, where they could proliferate and produce seen and palpable tumour deposits. These sites should be intentionally examined when looking for peritoneal metastases (Zonca et al 2008). The motion of peritoneal fluid explains the presence of disease at sites such as the undersurface of the proper hemidiaphragm and the pelvic pouches. An example is the Fitz�Hugh�Curtis syndrome, during which gonorrhoea or chlamydia organisms enter the peritoneal cavity via the uterine tubes and are transported within the peritoneal fluid to the best higher quadrant, where they trigger perihepatic inflammation. Direct communication of abdominal and pleural spaces known as pleuroperitoneal fenestrae may hardly ever exist (Pestieau et al 2000, Simmons and Mir 1989). The peritoneum is the biggest serous membrane within the body, and its arrangements are complex. Although its clean look is unremarkable, its construction is complicated and varies tremendously in different areas. Directly beneath the monolayer of mesothelium is a well-developed basement membrane, outside which is a wealthy lymphatic plexus. Microscopic mesothelial pores or peritoneal stomata are distributed all through the peritoneum however particularly on the undersurface of the diaphragm and anterior abdominal wall (Wassilev et al 1998). Neighbouring mesothelial cells are joined by junctional complexes but most likely allow the passage of macrophages. The submesothelial connective tissue may include macrophages, lymphocytes and adipocytes (in some regions). Mesothelial cells might rework into fibroblasts, which can play an necessary function in irritation of the peritoneum and the formation of peritoneal adhesions after surgery (Schn�riger et al 2011). The regular stress inside the peritoneal cavity is about 2�10 mmHg (higher in pregnancy and obese individuals) (Sanchez et al 2001). It can be measured immediately using a catheter inserted into the abdomen, or indirectly, by monitoring the strain within the bladder or abdomen. In such patients, monitoring of intraabdominal pressure can establish major will increase in strain (above about 25 mmHg) that could jeopardize the blood move to important organs and dictate the need for pressing decompression. The extraperitoneal tissue over the posterior stomach wall incessantly incorporates massive quantities of fats, especially in overweight males. The visceral peritoneum is firmly adherent to the underlying viscera and infrequently blends with connective tissue in the wall of the organ; it rarely incorporates loose connective or adipose tissue. The visceral peritoneum is often thought of as part of the underlying viscus for medical and pathological functions such because the staging of cancer. Because of its attachments, elimination of the parietal peritoneum within the management of peritoneal metastases is possible with out resection of underlying tissues, whereas cancer deposits on visceral peritoneum often require partial resection of the viscus for full removal (see Video sixty three. It accommodates a small amount of peritoneal fluid that not often exceeds 5 ml in healthy males and postmenopausal females (Yoshikawa et al 2013). In wholesome younger females, up to 25 ml of fluid could also be present, relying on the section of the menstrual cycle (Koninckx et al 1980). The fluid lubricates the cell viscera, permitting them to glide freely on the stomach wall and towards one another within the limits imposed by their attachments. However, the parietal peritoneum could be surgically removed with out necessarily having adverse effects on gut function (Sugarbaker 2012). Normal peritoneal fluid contains water, proteins (less than 30 g of protein per litre), electrolytes and solutes derived from interstitial fluid within the adjacent tissues and from plasma in native capillaries. It additionally incorporates a couple of cells, including desquamated mesothelium, nomadic peritoneal macrophages, mast cells, fibroblasts, lymphocytes and other leukocytes. Macrophages migrate freely between the peritoneal cavity and the encompassing connective tissue. In females, blood or fluid might enter the peritoneal cavity from a ruptured ovarian follicle (mittelschmerz) or from the retrograde move of menstrual fluid along the uterine tubes (which might trigger endometriosis). Peritoneal fluid gravitates to dependent websites inside the peritoneal cavity; diaphragmatic respiratory movements, adverse intrathoracic strain and intestinal peristalsis encourage flow from the pelvis to the subphrenic areas, even when the individual is erect. Ultimately, the ventral mesentery is basically resorbed, although some parts persist in the higher stomach and form buildings such because the lesser omentum and falciform ligament. The mesenteries of the intestines in the grownup are the remnants of the dorsal mesentery. These are all coated by visceral peritoneum, which is steady with the parietal peritoneum masking the posterior stomach wall. The first intraperitoneal loop is fashioned by the belly oesophagus, abdomen and first part of the duodenum. The second loop is made up of the duodenojejunal junction, jejunum, ileum and normally the caecum. The third loop contains the transverse colon, and the final loop contains the sigmoid colon and sometimes the distal descending colon. Left subphrenic space Arrows indicate the flow of Right subphrenic area Left triangular ligament Brown, Office of Visual Media peritoneal fluid. All however the higher omentum are composed of two layers of visceral peritoneum separated by variable quantities of fatty connective tissue. The greater omentum is folded again on itself and therefore consists of four layers of visceral peritoneum separated by variable quantities of adipose tissue. The mesenteries include the neurovascular bundles and lymphatic channels that supply the suspended organs.
Generic 80mg tadapox free shippingRelations the brachial artery is wholly superficial erectile dysfunction herbal supplements buy 80mg tadapox mastercard, coated anteriorly only by pores and skin and superficial and deep fasciae erectile dysfunction nervous tadapox 80 mg for sale. The bicipital aponeurosis crosses it anteriorly at the elbow erectile dysfunction statistics us cheap 80 mg tadapox with mastercard, separating it from the median cubital vein; the median nerve crosses it lateromedially near the distal attach ment of coracobrachialis diabetic erectile dysfunction pump buy discount tadapox on line. Posterior to the artery are the lengthy head of triceps, separated by the radial nerve and profunda brachii artery, and then successively by the medial head of triceps, the attachment Superior transverse scapular ligament Suprascapular artery Branches the branches of the brachial artery are the profunda brachii, nutrient, superior, middle and inferior ulnar collateral, deltoid, muscular, radial and ulnar arteries. This injury is associated with infraclavicular brachial plexus traction lesions (Birch 2011). The axillary artery provides the muscles of the ventral compartments of the shoulder, including the pectoral�deltoid muscle sheet, the scapulo humeral muscles (other than the posterosuperior rotator cuff) and the shoulder joint, including the scapula (with the serratus muscles) and proximal humerus. Its terminal branch, the brachial artery, supplies the muscular tissues of the anterior compartment of the arm (for the branches of the brachial artery at the elbow and in the forearm, see pages 856�858); the profunda brachii artery, the main proximal department of the brachial artery, supplies the muscle tissue of the posterior compartment of the arm and the shaft of the humerus. It follows the radial nerve intently, at first posteriorly between the long and medial heads of triceps, then within the spiral groove lined by the lateral head of triceps. The radial collateral department pierces the lateral intermuscular septum to reach the anterior facet of the epicondyle of the humerus in the groove between brachioradialis and brachialis, and takes half within the anastomosis around the elbow. The profunda brachii might originate from a typical origin with the posterior circumflex humeral artery, from the axillary artery proximal to the tendon of latissimus dorsi, or from the distal portion of the axil lary artery. Middle collateral (posterior descending) department the center collat eral artery is the larger terminal department of the profunda brachii artery. It arises posterior to the humerus and descends along the posterior surface of the lateral intermuscular septum to the elbow. Proximally, the artery lies between brachialis (anteriorly) and the lateral head of triceps (posteriorly). Distally, it lies between brachioradialis (anteriorly) and the lateral head of triceps (posteriorly). It might pierce the deep fascia and turn into cutaneous, or stay deep to the fascia till it anastomo ses with the interosseous recurrent artery behind the lateral epicondyle; it gives off about 5 small fasciocutaneous perforators and often has a small branch that accompanies the nerve to anconeus. It provides brachialis, brachioradialis, the radial nerve and a few fasciocutaneous perforators. It begins at the decrease border of teres major and ascends to the outer border of the primary rib, where it becomes the subclavian vein. It is joined by the brachial vein close to subscapularis, and by the cephalic vein near its costal end; different tributaries comply with the axillary arterial branches. The medial pectoral nerve, medial cord of the brachial plexus, ulnar nerve and medial cutaneous nerve of the forearm lie between the artery and the vein. The medial cutaneous nerve of the arm is medial to the vein; the lateral group of axillary lymph nodes is posteromedial. There are a pair of valves near its distal end, and valves also happen close to the ends of the cephalic and subscapular veins. It extends from the outer border of the primary rib to the medial border of scalenus anterior, the place it joins the internal jugular to type the bra chiocephalic vein. The clavicle and subclavius are anterior; the subcla vian artery is posterosuperior, separated by scalenus anterior and the phrenic nerve; and the first rib and pleura are inferior. Its tributaries are the external jugular, dorsal scapular and (sometimes) anterior jugular veins, and, often, a small branch from the cephalic vein that ascends anterior to the clavicle. Brachial veins the brachial veins flank the brachial artery, as venae comitantes with tributaries much like the arterial branches; they be part of the axillary vein near the decrease margin of subscapularis. The medial branch typically joins the basilic vein earlier than it becomes the axillary vein. It accompanies the ulnar nerve, piercing the medial intermuscular septum to descend within the posterior compartment and provide the medial head of triceps. It passes between the medial epicondyle and olecranon, ending deep to flexor carpi ulnaris by anas tomosing with the posterior ulnar recurrent and inferior collateral arter ies. A department generally passes anterior to the medial epicondyle and anastomoses with the anterior ulnar recurrent artery. Entering the infra clavicular fossa to pass posterior to the clavicular head of pectoralis main, it pierces the clavipectoral fascia, crosses the axillary artery and joins the axillary vein just below clavicular stage. It may join with the external jugular vein by a department anterior to the clavicle. Sometimes, the median cubital vein is massive, transferring most blood from the cephalic to the basilic vein, by which case the proximal cephalic vein is both absent or a lot diminished. Middle ulnar collateral artery If present, the middle ulnar col lateral artery arises from the brachial artery between the superior and inferior ulnar collateral arteries. It passes anterior to the medial epi condyle and anastomoses with the anterior ulnar recurrent artery. By its junction with the middle collateral department of the profunda brachii artery, it types an arch proximal to the olecranon fossa. As it lies on brachialis, it offers off branches that descend anterior to the medial epicondyle to anastomose with the anterior ulnar recurrent artery. Behind the epicondyle, a branch anastomoses with the superior ulnar collateral and posterior ulnar recurrent arteries. In the axilla, the lateral and posterior cords of the brachial plexus are anterior and lateral to the primary part of the axillary artery, respectively, and the medial cord is behind the artery. The cords assume their appro priate relations around the second a part of the artery, deep to pectoralis main. Other than the medial root of the median Muscular branches Muscular branches are distributed to coraco brachialis, biceps and brachialis. Deltoid (ascending) branch the deltoid department ascends between the lateral and long heads of triceps, and anastomoses with a descending branch of the posterior humeral circumflex artery. Radial and ulnar arteries the radial and ulnar arteries are described in detail on web page 856 and 857, respectively. Anterior to the artery, it joins a ramus of the lateral pectoral nerve and enters the deep surface of pectoralis minor, which it supplies. Two or three branches pierce pectoralis minor and others might pass round its inferior border to end in pectoralis major. Upper (superior) subscapular nerve Intercostobrachial nerve Medial cutaneous nerve of arm Cephalic vein the superior subscapular nerve is smaller than the inferior. It arises from the posterior cord (C5, 6), enters subscapularis at a excessive stage, and is incessantly double. Lower (inferior) subscapular nerve the inferior subscapular nerve arises from the posterior wire (C5, 6). It supplies the lower part of subscapularis and ends in teres main, which is sometimes supplied by a separate branch. Thoracodorsal nerve the thoracodorsal nerve arises from the posterior twine (C6�8) between the subscapular nerves. It is, at first, lateral to the radial nerve, posterior to the axillary artery and anterior to subscapularis. At the decrease border of subscapularis, it curves again inferior to the humeroscapular articular capsule and, with the posterior circumflex humeral vessels, traverses a quadrangular house bounded above by subscapularis (anteriorly) and teres minor (posteriorly), beneath by teres major, medially by the long head of triceps, and laterally by the surgical neck of the humerus. The anterior department curves round the neck of the humerus with the posterior cir cumflex humeral vessels, deep to deltoid, to attain the anterior a half of the muscle. At the level of the anterior border of the acromion, the nerve often consists of two or extra thin filaments that provide the anterior deltoid; it gives off a couple of small cutaneous branches that pierce deltoid and ramify in the pores and skin over its decrease half. The posterior department programs medially and posteriorly along the attachment of the lateral head of triceps, inferior to the glenoid rim. It offers off the nerve to teres minor and the higher lateral cutaneous nerve of the arm at the lateral fringe of the attachment of the lengthy head of triceps. The posterior department regularly supplies the posterior facet of deltoid, often through a separate branch from the principle stem, but sometimes from the superior lateral cutane ous nerve of the arm. However, the posterior a part of deltoid has a extra consistent supply from the anterior branch of the axillary nerve, which should be remembered when performing a posterior deltoidsplitting method to the shoulder. The upper lateral cutaneous nerve of the arm pierces the deep fascia on the medial border of the posterior aspect of deltoid, and provides the pores and skin over the lower a half of deltoid and the higher part of the lengthy head of triceps. The posterior department is intimately related to the inferior elements of the glenoid and shoulder joint capsule. It runs laterally, deep to trapezius and omohy oid, and enters the supraspinous fossa via the suprascapular notch inferior to the superior transverse scapular ligament. It runs deep to supraspinatus, supplies it, and curves round the lateral border of the spine of the scapula with the suprascapular artery to attain the infrasp inous fossa, where it gives two branches to infraspinatus and articular rami to the shoulder and acromioclavicular joints. When current, it pierces deltoid near the tip of the acromion and supplies the pores and skin of the proximal third of the arm within the territory of the axillary nerve. Lateral pectoral nerve the lateral pectoral nerve (C5, 6) is bigger than the medial, and will arise both from the anterior divisions of the upper and middle trunks, or by a single department from the lateral cord, just above or deep to the clavicle.
Buy tadapox cheap onlineThe root of the mesentery of the small intestine is continuous with the peritoneum that surrounds the appendix and caecum in the proper iliac fossa impotence jelly order tadapox 80mg with visa. Umbilicus Posterior layer of rectus sheath Arcuate line Inferior epigastric vessels Testicular vessels External iliac artery and vein Lateral inguinal fossa Medial inguinal fossa Supravesical fossa Urinary bladder Mesoappendix the mesentery of the appendix is a fatty impotence injections medications order tadapox from india, triangular fold of peritoneum that passes between the posterior floor of the mesentery of the terminal ileum near what std causes erectile dysfunction purchase 80 mg tadapox fast delivery the ileocaecal junction and the vermiform appendix diabetes-induced erectile dysfunction epidemiology pathophysiology and management order 80 mg tadapox otc. It may end wanting the tip of the appendix, during which case a thin, shallow fold of peritoneum containing fat is current in course of the tip. It encloses the blood vessels, nerves and lymph vessels of the vermiform appendix, and usually accommodates a lymph node. Medial umbilical fold Median umbilical fold Ureter Vas deferens Sigmoid mesocolon the sigmoid mesocolon varies in size and depth between individuals. The left limb of the attachment runs over the left psoas main and alongside the exterior iliac vessels. The proper limb passes over the pelvic brim towards the midline at the stage of the third sacral vertebra. The anteromedial peritoneal layer of the sigmoid mesocolon is continuous with the peritoneum of the lower left posterior belly wall, and its posterolateral layer is steady with the peritoneum of the lateral stomach wall. Bands of peritoneum could also be present running from the proximal sigmoid colon to the posterior abdominal wall. The sigmoid and superior rectal vessels run between its layers and the left ureter descends into the pelvis behind its apex and anterior to the bifurcation of the left widespread iliac artery. The median umbilical fold extends from the umbilicus to the apex of the bladder and accommodates the urachus or its remnant (Ch. The medial umbilical fold overlies the obliterated umbilical artery, which ascends from the interior iliac artery within the pelvis to the umbilicus. The lateral umbilical fold covers the inferior epigastric vessels below their entry into the rectus sheath. The supravesical fossa lies between the medial and median umbilical folds on both sides of the midline, and the medial and lateral inguinal fossae lie on both side of each lateral umbilical fold. The lateral inguinal fossa overlies the deep inguinal ring, and the medial inguinal fossa overlies the femoral ring (Healy and Reznek 1999). The pouch is limited laterally by sacrogenital folds of peritoneum, which prolong posteriorly from the edges of the bladder to the anterior side of the sacrum. When the bladder is empty, a transverse vesical fold could additionally be visible at laparoscopy; its medial portion overlies the superior vesical artery or arteries (Boaz et al 2011). Between the paravesical and pararectal fossae, the ureters and inside iliac vessels may trigger slight elevations within the peritoneum. From the apex of the bladder, the median umbilical fold extends superiorly on the posterior floor of the decrease anterior abdominal wall to the umbilicus. When the bladder distends, the overlying peritoneum is lifted in order that a part of the anterior floor of the bladder comes into direct contact with the posterior surface of the lower anterior belly wall. This signifies that a distended bladder could be punctured instantly via the lower anterior belly wall with out traversing the peritoneal cavity (suprapubic puncture). Peritoneum of the female pelvis In females, peritoneum covers the anterolateral floor of the higher rectum because it does within the male, nevertheless it descends further over the anterior floor of the rectum. The presence of the uterus and vagina means that there are two pelvic pouches instead of the one rectovesical pouch seen in males. The peritoneum from the rectum is reflected anteriorly on to the posterior surface of the posterior fornix of the vagina and the uterus, forming the recto-uterine pouch (of Douglas). The depth of the pouch � specifically, the extent to which it descends on the posterior surface of the vagina � is variable (Baessler and Schuessler 2000). As in males, the peritoneum over the dome of the bladder is mirrored on to the posterior surface of the lower anterior stomach wall. Recto-uterine folds containing the uterosacral ligaments move posteriorly from the edges of the cervix to the sacrum, running lateral to the rectum. This consists of anterior and posterior layers which are steady at the upper border of the ligament. The broad ligament accommodates the uterine tubes in its free upper border; the ovaries are suspended from its posterior layer. The ovarian fossa is a shallow despair within the peritoneal lining of the lateral pelvic wall between the peritoneal ridges fashioned by the obliterated umbilical arteries anteriorly, the ureter posteriorly, and the external iliac vessels above; it lies behind the lateral attachment of the broad ligament and usually contains the ovary in nulliparous females. Parietal peritoneum is equipped by the somatic blood vessels of the stomach and pelvic walls, and its lymphatics join these in the body wall and drain to parietal lymph nodes. Visceral peritoneum is finest thought-about as an integral part of the viscus it covers: its blood supply and lymphatic drainage therefore correspond to these of the related viscus. Pain from the pancreas, gallbladder and even the small bowel could radiate to the again. Stretch or irritation of the visceral peritoneum can also elicit profound reflex vasomotor and cardiac modifications mediated by autonomic nerves, including a vasovagal response. Painful responses to manipulation of the parietal peritoneum may be abolished by native or regional anaesthesia. In marked distinction, the direct central connections of visceral afferents, particularly through the vagus nerve, mean that stretching the visceral peritoneum may induce profound results, including acute haemodynamic instability, despite native or regional (including spinal) anaesthesia. It consists of the greater sac, which is the primary peritoneal cavity surrounding many of the abdominal and pelvic viscera, and the lesser sac, or omental bursa, which is a small diverticulum located behind the stomach and lesser omentum and in front of the pancreas. It is beneficial to divide the peritoneal cavity into two primary compartments, supramesocolic (often merely known as supracolic) and inframesocolic (or infracolic), that are partially separated by the transverse colon and its mesentery. The visceral peritoneum is innervated by afferent nerves that travel with the autonomic supply to the underlying viscera. Sensations arising from pathologies that affect the parietal or visceral peritoneum replicate these completely different patterns of innervation. Well-localized pain is elicited by mechanical, thermal or chemical stimulation of nociceptors within the parietal peritoneum; the ache is often nicely localized to the affected region. Somatic nerves that innervate the parietal peritoneum additionally provide the corresponding segmental pores and skin and muscle tissue; when the parietal peritoneum is irritated, native reflex muscle contraction occurs, resulting in scientific indicators of guarding and even rigidity of the abdominal wall. The parietal diaphragmatic peritoneum is equipped centrally by afferent fibres from the phrenic nerves and peripherally by the lower intercostal and subcostal nerves; peripheral irritation of the diaphragm could therefore end in ache localized in the distribution of the lower thoracic spinal nerves, whereas central irritation causes referred ache within the cutaneous distribution of the third to fifth cervical spinal nerves (the shoulder region). The innervation of the parietal peritoneum of the true pelvis is poorly documented however the obturator nerve makes a major contribution. Irritation or stretch of the visceral peritoneum causes poorly localized discomfort. The right supramesocolic house may be subdivided into the proper subphrenic house, the right subhepatic area and the lesser sac. The left supramesocolic space can be divided into two subspaces: the left subphrenic area and the left perihepatic area. Right subhepatic house (hepatorenal pouch) the right subhepatic house lies between the inferior floor of the best lobe of the liver and the upper pole of the best kidney. It is bounded superiorly by the inferior layer of the coronary ligament, laterally by the right lateral abdominal wall, posteriorly by the anterior surface of the higher pole of the proper kidney, and inferomedially by the hepatic flexure, transverse mesocolon, second part of the duodenum, and part of the head of the pancreas. In the supine position, the hepatorenal pouch (of Morison) is extra dependent than the right paracolic gutter. Lesser sac (omental bursa) the lesser sac is a cavity lined with peritoneum and linked to the primary peritoneal cavity (greater sac) by the epiploic foramen (of Winslow). It is considered a half of the proper supramesocolic compartment as a result of it develops in the embryo on the right side of the ventral mesogastrium (p. It has posterior and anterior partitions and superior, inferior, right and left borders. The sac varies in dimension according to the amount of the viscera making up its partitions; it may be partially obliterated by pure adhesions between the anterior and posterior walls. At its proper border, the anterior wall is usually fashioned by the lesser omentum but, in path of the left, the lesser omentum becomes progressively shorter and extra of the anterior wall is shaped by the posterior floor of the abdomen and greater omentum. The lower a half of the posterior wall of the lesser sac is formed by the anterior peritoneal layer of the posterior sheet of the greater omentum, which overlies the transverse mesocolon. The inferior phrenic, splenic, left gastric and customary hepatic arteries lie partly behind the bursa. Here, the peritoneum of the posterior wall of the lesser sac is mirrored anteriorly from the diaphragm to join the posterior layer of the lesser omentum.
Syndromes - Rubbing alcohol
- Cramps for a week or two before menstruation and during menstruation; cramps may be steady and range from dull to severe)
- Changes in organ function
- A mental status examination
- Has a fever that does not go down with acetaminophen (Tylenol) or ibuprofen (Advil) and a cool bath
- Nervousness, irritability, moodiness, or sleeplessness that is new or getting worse
- Mushrooms
- Over-inflation of a part of the lungs (emphysema can cause this)
- Poor eating habits (babies may get tired while nursing or sweat during feedings)
Buy generic tadapox 80 mg on-lineBasal chordae erectile dysfunction doctors in brooklyn purchase tadapox with mastercard, in distinction erectile dysfunction nyc buy generic tadapox on line, are solitary constructions passing from the ventricular wall to the mural leaflet zma erectile dysfunction discount tadapox 80 mg overnight delivery. There is such marked variation between the arrangement of the chordae that any detailed classification loses much of its scientific significance erectile dysfunction brands 80mg tadapox visa. Note how the supporting sinuses could also be described as left coronary, right coronary and non-adjacent, based on the origin of the coronary arteries. Note the inter-leaflet triangles, membranous septum, and fibrous continuity between the aorta and mitral valve. Chordae tendineae come up mostly from the tip and apical third of every muscle but typically take origin close to their base. The chordae from every papillary muscle diverge and are connected to corresponding areas of closure on each valvular leaflets. As such, it possesses important length, however due to the semilunar attachment of the leaflets, it has no discrete proximal border. The muscular portion of the aortic root is roughly two-thirds of its widest circumference. Descriptions of the aortic root over the years have been bedevilled by accounts of a valve anulus. There are at least two rings throughout the root; neither serves to support the valve leaflets, that are attached in semilunar trend from the sinutubular junction to a basal ventricular attachment. Two leaflets are supported by muscle, and the third has an solely fibrous attachment. The root acts as a bridging construction not only anatomically, separating the myocardial and arterial parts of the left ventricular pathway, but also functionally as a end result of its proximal and distal elements can face up to appreciable adjustments in ventricular and arterial pressures. The fibrous core that flanks each nodule is tenuous, forming the lunules of translucent and sometimes fenestrated valvular tissue; fenestrations are of no useful significance. Posterior, right and left refer to their fetal positions before full cardiac rotation has occurred (Ch. Corresponding phrases based on their approximate positions in maturity are anterior, left and proper posterior. Aortic sinuses (of Valsalva) the aortic sinuses are extra distinguished than those within the pulmonary trunk. Coronary arteries usually open close to this ridge inside the higher part of the sinus however are markedly variable of their origin. The walls of the sinuses are largely collagenous near the attachment of the leaflets but the amount of lamellated elastic tissue will increase with distance from the zone of attachment. At the midlevel of every sinus, its wall is about half the thickness of the supravalvular aortic wall and fewer than one-quarter of the thickness of the sinutubular ridge. At this level, the mean luminal diameter on the commencement of the aortic root is way bigger than that of the ascending aorta; these particulars are functionally vital within the mechanism of valvular motion. A linear relationship between the diameter of the aortic sinus and the square root of body surface area has been described in kids (Kaiser et al 2008). The three nodules are apposed and the margins and lunular elements of adjacent leaflets are tightly apposed on their ventricular elements. As ventricular systolic strain will increase, it exceeds aortic pressure and the valve is passively opened. The fibrous wall of the sinuses nearest the aortic vestibule is almost inextensible but, extra superiorly, the wall is fibroelastic. Under left ventricular ejection stress, the radius right here will increase 16% in systole, as the commissures transfer aside to form a completely open triangular orifice. The free margins of the leaflets then turn out to be nearly straight lines between peripheral attachments. Tight and full closure ensues with the rapid lower in ventricular stress in diastole. Commissures slender, nodules mixture and the valve reassumes its triradiate form. Experiments point out that 4% of ejected blood regurgitates via a valve with regular sinuses, whereas 23% regurgitates via a valve without them. The regular structure of the aortic sinuses also promotes nonturbulent flow into the coronary arteries. Aortic valve leaflets the aortic valve leaflets are connected partly to the aortic wall and partly to the supporting ventricular buildings. As with the pulmonary valve, the semilunar attachments incorporate segments of ventricular tissue throughout the bases of two of the aortic sinuses. However, the so-called non-coronary leaflet is better termed the non-adjacent leaflet as a result of it not often gives rise to a coronary artery. The semilunar attachments incorporate three triangular areas (trigones) of aortic wall throughout the apex of the left ventricular outflow tract. They are interposed between the bulbous aortic sinuses and separate the cavity of the left ventricle from the pericardial space. Removal of the trigones in an in any other case intact coronary heart is instructive in demonstrating the relationships of the aortic valve, which, justifiably, may be thought of because the keystone of the center. The first triangle, between the non-coronary and left coronary leaflets, has a base steady inferiorly with the fibrous aortic�mitral curtain. Although the basal attachments of every aortic valvular leaflet are thickened and collagenous at their ventricular origins, the leaflets lack a steady collagenous circular skeletal help; valvular operate relies upon primarily upon the semilunar attachments of the leaflets. With the valve half-open, each equals slightly greater than 1 / 4 of a sphere, an approximate hemisphere being accomplished by the corresponding sinus. Angling the beam in the path of the best additionally permits assessment of the best atrium, proper ventricle and tricuspid valves. The hinge of the leaflet is well below the extent of the ventriculoarterial junction. The muscular tissue of the ventricle is stained pink; fibrous tissue, which would present up as a attribute light colour with this stain, is absent. Note three aortic leaflets � right, left and non-adjacent � and the central place of the aorta. Note the totally different orientation compared with transthoracic echocardiography (looked at from below, foot to head). Rotation of the transducer permits two-chamber views of the guts and more detailed evaluation of the aorta and aortic valves. Over much of the center, a fine layer of areolar tissue is discovered beneath the mesothelium of the serous (visceral) epicardium that accumulates subepicardial fat, concentrated along the acute margin, the atrioventricular and interventricular grooves, and their aspect channels. The coronary vessels and their major branches are embedded on this fats; the amount will increase with age. Fibrocellular elements of those subepicardial and subendocardial layers mix on their mural features with the endomysial and perimysial connective tissue on the myocardium. Each cardiac myocyte is invested by a delicate endomysium composed of fantastic reticular, collagen and elastin fibres embedded in ground substance. This matrix is lacking solely at desmosomal and gap junctional contacts of intercalated discs. Similar arrangements apply to ventricular conduction myocytes and their extensive working myocardial contacts. The 1012 connective tissue matrix itself is interconnected laterally to type bundles, strands or sheets of macroscopic proportions exhibiting a posh geometric sample. Surrounding and attaching to bigger myocardial bundles are stronger perimysial condensations. Running at the ventricular base is a complex framework of dense collagen with membranous, tendinous and fibroareolar extensions, intimately associated to atrioventricular valves and the aortic orifice. The leaflets of the pulmonary valve are supported on a free-standing sleeve of right ventricular infundibulum that can easily be faraway from the heart without disturbing either the fibrous skeleton or the left ventricle. Two pairs of curved, tapering, collagenous prongs, fila coronaria, prolong from the central fibrous body. They are stronger on the left, the place they pass partially around the mitral and tricuspid orifices. In distinction, the aortic valve faces superiorly, mendacity anterosuperior and to the right of the mitral orifice. The two ends of the curtain are strengthened as the best and left fibrous trigones, that are the strongest parts of the skeleton. The right trigone, along with the membranous septum, constitutes the central fibrous 7 Heart body, which is penetrated by the atrioventricular bundle of His (see below). The membranous septum is crossed on its right side by the attachment of the tricuspid valve, dividing the septum into atrioventricular and interventricular parts. However, as with the pulmonary valve, the structure of the aortic root corresponds to the triple fibrous semilunar attachments of its leaflets.
Cheap 80mg tadapox overnight deliveryEach semilunar leaflet is contained inside one of many three sinuses of the pulmonary trunk erectile dysfunction doctor in dubai purchase 80mg tadapox fast delivery. This surface ends on the shallow vertical interatrial groove that descends to the cardiac crux impotence may be caused from quizlet best order for tadapox. The left atrial appendage is characteristically longer erectile dysfunction newsletter buy genuine tadapox online, narrower and more hooked than the right what causes erectile dysfunction yahoo 80 mg tadapox, and is a finger-like extension with more deeply indented margins. It is constricted at its atrial junction and all its contained pectinate muscles are a lot smaller than their proper counterparts. The left atrium lacks a crista terminalis, and the muscle bundles within the appendage are organized in a whorl-like style rather than being in an array. Its narrow morphology renders the left atrial appendage a possible site for deposition of thrombi. Their orifices are smooth and oval, the left pair incessantly opening by way of a common channel. Interpulmonary ridges are usually found between ipsilateral orifices; probably the most prominent is located between the openings of the left atrial appendage and left superior pulmonary vein. The ridges are infoldings of the left atrial wall and contain adipose tissue, atrial arteries and nerve bundles. At the positioning of the pericardial reflection, the atrial musculature extends into the pulmonary veins, forming myocardial sleeves which are thickest in the inferior wall of the superior pulmonary veins and the superior walls of the inferior pulmonary veins. They lie external to the venous tunica media and inside to the epicardium/ adventitia and are often the site of focal electrical exercise that initiates atrial fibrillation. Atrial myocardial bridges and crossing strands are sometimes present, connecting the left superior and inferior pulmonary veins. Several epicardial fat pads on the pulmonary venous component house the superior left, posterolateral, left inferior and posteromedial ganglionated cardiac intrinsic nerve plexuses (typically four). Minimal cardiac veins (venae cordis minimae) return blood instantly from the myocardium to the left atrial cavity. The left atrial facet of the septum has a characteristically rough appearance, bounded by a crescentic, superiorly concave ridge that marks the site of the foramen ovale. The musculature between the ostium of the inferior pulmonary vein and the Opening of the pulmonary valve During diastole, all three leaflets of the pulmonary valve are tightly apposed. The pulmonary valve is troublesome to visualize at echocardiography and usually solely the posterior leaflet is visible when the valve is closed; atrial systole could cause a slight posterior motion of the valve leaflets. Left atrium General, exterior and inside options Although smaller in quantity than the proper, the left atrium has thicker partitions (3 mm on average). It possesses a venous component that receives the best and left superior and inferior pulmonary veins, a vestibule and an appendage. Its cavity and walls are fashioned largely by the proximal elements of the pulmonary veins that are integrated into the atrium throughout development. Its intensive body is a remnant of the preliminary atrial element of the primary heart tube. The left atrium is roughly cuboidal, extending posterior to the right atrium and separated from it by the obliquely positioned septum. The left part is hid anteriorly by the initial segments of the pulmonary trunk and aorta: a part of the transverse pericardial sinus lies between it and these arterial trunks. Anteroinferiorly, and to the left, it adjoins the bottom of the left ventricle on the orifice of the mitral valve. Perspective causes the pulmonary anulus to appear smaller than the aortic anulus, whereas, actually, the reverse is the case. The impact of obesity on the heart is obvious as early as the second yr of life. Obese kids aged 2 years have a greater left ventricular mass in contrast with regular weight controls (de Jonge et al 2011). Left ventricle General and external features the left ventricle is constructed in accordance with its function as a robust pump for the high-pressured systemic arterial circulation. It types a part of the sternocostal, left and inferior (diaphragmatic) cardiac surfaces. The anterior and posterior (inferior) interventricular grooves indicate the lines of mural attachment of the ventricular septum and the limits of the ventricular territories. The sternocostal surface of the ventricle curves bluntly into its left surface at the obtuse margin. The shape of the left ventricle changes from elliptical within the neonatal interval to the spherical adult shape later in infancy (Azancot et al 1983). Internal options 1006 the left ventricle has an inlet region guarded by the mitral valve (ostium venosum), an outlet region guarded by the aortic valve (ostium arteriosum) and an apical trabecular part. After closure of the mitral leaflets and all through the ejection phase of systole, blood is expelled from the apex via the aortic orifice. Towards the aortic orifice, the septum turns into the skinny and collagenous interventricular part of the membranous septum, an oval or spherical area beneath and confluent with the fibrous triangle separating the best and the non-coronary leaflets of the aortic valve. Between the inferior limits of the free margins of the leaflets of the mitral valve and the ventricular apex, the muscular partitions exhibit deeper, finer and extra intricate trabeculae carneae than these of the best ventricle, characteristically extra developed nearer the apex, and becoming smoother as the superior septal surface is reached. A, the oesophagus (O) passing behind the posterior left atrial wall and a broad left-lateral ridge (double-headed arrow). B, the section passes via the os of the left atrial appendage and the infolding of the ridge. The triangle signifies the carina or interpulmonary ridge between the higher and decrease pulmonary veins. Thus it has an orifice with a supporting anulus, leaflets and a selection of chordae tendineae and papillary muscular tissues. Mitral valvular orifice the mitral orifice is a well-defined transitional zone between the atrial wall and the leaflet bases, being smaller than the tricuspid orifice (mean circumference is 9. The roughly round orifice is kind of vertical and at 45� to the sagittal aircraft in diastole, but with a slight anterior tilt. Its ventricular facet faces anterolaterally to the left and slightly inferiorly in path of the left ventricular apex. The mitral, tricuspid and aortic orifices are intimately connected at their central fibrous physique. When the mitral valve leaflets close, they kind a single zone of coaptation, termed the commissure. Note the relationship of the leaflet insertions and the ventriculoarterial junction. C, the foundation of the aorta has been minimize open and distended, so as to show the insertion of the semilunar leaflets. Note the zone of fibrous continuity between the leaflets of the aortic and mitral valves and their relationship to the fibrous trigones, and the semilunar attachment of the leaflets (compare with B). Echocardiography precisely assesses the degree of thickening and its effect on systolic function, similar to dynamic left ventricular outflow obstruction, systolic anterior movement of the aortic mitral valve leaflet and mid-systolic closure of the aortic valve. A number of histological changes are observed, together with cardiomyocytic disarray with substitute fibrosis and collagenous part enlargement. Treatment is often medical, apart from refractory instances and those in whom the left ventricular outflow tract obstruction has a gradient of greater than 50 mmHg. Catheter alcohol septal ablation has been introduced as a non-surgical various. A number of patients may also require implantation of cardiac defibrillators to prevent sudden cardiac death. In distinction, hypertrophic cardiomyopathy reveals asymmetric patterns of left ventricular hypertrophy, often with sharp segmental transitions, left atrial enlargement and weird electrocardiographic patterns. The smooth-walled venous component of the left atrium is probably the most extensive component. The septal aspect of the left atrium exhibits the crescentic line of the free edge of the flap valve in opposition to the rim of the fossa ovalis. The orifices of the right superior and inferior pulmonary veins are adjoining to the plane of the septal facet of the left atrium. The anulus is strongest at the internal elements of the left and right fibrous trigones. Between the prong suggestions, the atrial and ventricular myocardial plenty are separated by a more tenuous sheet of deformable fibroelastic connective tissue. Mitral valve leaflets the mitral valvular leaflets have lengthy been described as paired buildings. Its free edge bears several indentations, of which two are sufficiently deep and common to be nominated as the ends of a solitary and indirect zone of apposition or 1008 commissure. These anteromedial (inferoseptal) and posterolateral (superoposterior) extremities may be regarded as two independent commissures, every positionally named as indicated in brackets.
Cheapest tadapoxThe appendicular vein usually joins the caecal vein to turn into the ileocolic vein; infection from the appen dix can subsequently be carried directly to benadryl causes erectile dysfunction buy cheap tadapox 80mg on line the liver through the portal vein whey protein causes erectile dysfunction order tadapox 80mg free shipping. Its place with respect to the spleen is variable: it usually lies inferomedial to the lower pole erectile dysfunction statistics cdc order cheapest tadapox, forming the colic impression erectile dysfunction what doctor to see purchase tadapox 80mg visa, but it could lie anterior to the splenic hilum, or even a little above. The splenic flexure is usually connected to the splenic capsule by a peritoneal ligament and inadvertent downward traction on the flexure during surgery may tear the splenic capsule. The phrenicocolic ligament attaches the flexure to the diaphragm under the inferior pole of the spleen at about the stage of the tenth rib. The splenic flexure usually adopts a very acute angle such that the top of the trans verse colon overlaps the beginning of the descending colon; there could the descending colon is 25�30 cm long and descends from the splenic flexure within the left hypochondrium to the extent of the iliac crest, the place it curves medially anterior to iliacus to turn out to be the sigmoid colon. Its lateral peritoneal reflection in the left paracolic gutter is marked by a white line (of Toldt). The subcostal vessels and nerves, iliohypogastric, ilioinguinal, lateral femoral cutaneous, femoral and genitofemoral nerves, and, usually, the fourth lumbar artery also lie posteriorly, and loops of jejunum are anterior. The descending colon is smaller in calibre and extra deeply placed than the ascending colon. Lymph drainage from the midgut follows the course of the superior mesenteric artery. When the distal transverse colon and splenic flexure are predominantly equipped by the middle colic artery, lymph drainage of this phase can additionally be largely to superior mesenteric nodes. Lymphatic vessels within the appendix are numerous and combine to kind vessels that ascend within the mesoappendix, often interrupted by one or more nodes. They unite to form three or four bigger vessels that anastomose with lymphatic vessels draining the ascending colon into ileocolic nodes. The mesocolon consists of fats embedded within a con nective tissue lattice and sandwiched between two layers of mesothelium; it also accommodates nerves, blood and lymphatic vessels, and lymph nodes. It is normally suspended from the posterior belly and pelvic walls by a fanshaped sigmoid mesocolon, however could also be tethered by congenital adhesions to the parietal peritoneum over iliacus. It usually lies inside the pelvic cavity anterior to the rectum on the peritoneal floor of the bladder (and uterus in the female). Later ally are the left external iliac vessels, the obturator nerve, ovary or vas deferens, and the lateral pelvic wall; posteriorly lie the left exterior and inner iliac and gonadal vessels, ureter, piriformis and the sacral plexus; anteroinferiorly lie the bladder in males, or the uterus and bladder in females; superiorly and to the right, the sigmoid colon is in contact with loops of the ileum. The gonadal vessels and ureter lie in a distinct fascial plane, which is the inferior extension of the retroperito neal perirenal fascia and is separate from the sigmoid mesocolon. This plane may be acknowledged and separated throughout surgical resection of the sigmoid mesocolon. The taeniae coli of the sigmoid colon are wider than elsewhere in the colon, and coalesce at its distal end to form a whole circumferential longitudinal muscle layer. The place and form of the sigmoid colon rely upon its size (which increases with age) and mobility; the length of the sigmoid mesocolon (usually longer in males); and the diploma of distension of the colon, rectum, bladder and uterus. The length of the sigmoid colon and its mesentery range between ethnic groups (Alatise et al 2013). It descends throughout the sacrococcygeal concavity, at first working posteriorly after which curving anteriorly. The junction between the ante riorly directed distal rectum and the posteriorly directed anal canal is the anorectal angle, which is maintained by puborectalis. This is 2�3 cm anterior to and barely beneath the tip of the coccyx, level with the apex of the prostate in males. The rectum additionally deviates in three lateral curves: higher, convex to the right; center (the most prominent), convex to the left; and lower, convex to the right. Although variable in absolute length, the rectum is often defined in scientific follow as extending roughly 15 cm above the exterior anal margin. Its upper diameter is similar to that of the sigmoid colon, however more inferiorly it becomes dilated as the rectal ampulla. Unlike the sigmoid colon, the rectum has no sacculations, appendices epiploicae or taeniae coli. The taeniae merge a quantity of centimetres above the recto sigmoid junction, initially forming extensive anterior and posterior muscu lar bands that then fuse to kind a continuous outer layer of longitudinal muscle investing the entire size of the rectum. At the rectal ampulla, a couple of longitudinal muscle fibres move forwards from the anterior rectal wall to the perineal physique and urethra (rectourethralis). The higher third of the rectum is roofed by peritoneum on its ante rior and lateral features, and the middle third by peritoneum on its anterior aspect only; the lower third is beneath the peritoneum. Volvulus is more doubtless when the size of the sigmoid colon and the length and width of its mesentery are higher (Akinkuotu et al 2011). The anatomical options predispos ing to sigmoid volvulus are mostly present in subSaharan Africans and chronically institutionalized sufferers. Acquired diverticula generally happen within the sigmoid colon, particu larly in Western populations. These diverticula frequently develop in parallel rows between the mesenteric taenia coli and the two anti mesenteric taeniae the place the colonic wall is weaker; at this site, the outer longitudinal muscle is deficient and the round muscle is tra versed by arteries supplying the submucosal vascular plexus (Slack 1962). However, the predilection of diverticula in the sigmoid colon most likely relates to causative factors quite than intrinsic variations in the construction of this phase of the colon. The level of this reflection is greater in males; the rectovesical pouch is approximately 7. In neonatal boys, the peritoneum extends on the anterior rectal wall as far as the lower limit of the prostate. When the rectum is empty, the mucosa has a quantity of longitudinal folds in its decrease half, which turn out to be effaced during distension. One consists of the mucosa, the round muscle layer and a part of the longitudinal muscle, and is marked externally by an indenta tion. The most superior fold at the beginning of the rectum may be on both the left or the right and occasionally encircles the rectal lumen. The middle fold is largest and most constant, and lies immedi ately above the rectal ampulla, projecting from the anterior and proper wall just below the level of the anterior peritoneal reflection; the round muscle is especially distinguished on this fold. Relations Posterior to the rectum and mesorectum, separated by the presacral fascia, are the lower three sacral vertebrae, coccyx, median and lateral sacral vessels, and the bottom portion of the sacral sympathetic chain. Laterally, the upper rectum is expounded to the sigmoid colon and/ or small bowel, while beneath the peritoneal reflection lie levator ani, obturator internus, the obturator nerve and vessels, ureters, the inferior hypogastric plexus, inner iliac vessels, piriformis and the sacral plexus. In females, the cervix/body of the uterus and vagina are anterior, the latter separated from the rectum by a rectovagi nal septum. In postmenopausal females, and after childbirth, the con nective tissue of the rectovaginal septum might atrophy or turn into thinned, lowering the support of the anterior rectal and posterior vaginal partitions. It incorporates the superior rectal artery and its branches, the superior rectal vein and its tributaries, lymphatic vessels and nodes, and adipose connective tissue. The latter is a skinny layer of connective tissue that passes obliquely downwards from the presacral fascia to fuse with the mesorectal fascia posterior to the rectum 3�5 cm above the anorectal junction (Garc�aArmengol et al 2008). The mesorectal fascia is sur rounded by a skinny and relatively avascular layer of loose areolar tissue, which separates it from the posterior and lateral partitions of the true pelvis. Superiorly, the mesorectal fascia blends with the connective tissue bounding the sigmoid mesentery. This fascia is typically confusingly often identified as rectovesical fascia in males however it extends caudal to the bladder and is particularly dense posterior to the prostate and seminal vesicles; it lies immediately anterior to the mesorectal fascia, to which it might be fused (Lindsey et al 2000). Identification of this layer in patients with a malignant rectal tumour might help predict the success of surgical resection. Branches of the inferior hypogastric plexus and middle rectal vessels enter the mesorectum anterolaterally. The number and calibre of the center rectal vessels are highly variable; they might be very small or even absent (Sato and Sato 1991). Descent occurs within the lumen of the rectum as a form of intussusception, and could also be a consequence of the big diameter of the rectal ampulla and relative fixation of the anal canal. Chronic enlargement of the anorectal space certain by levator ani commonly happens in sufferers suffering from recur rent rectal prolapse, however is probably a consequence somewhat than a reason for the prolapse. When the rectovaginal septum is grossly effaced, particularly in publish menopausal females, the pressure of defecation may cause bulging of the rectal wall into the posterior vagina and, in extreme cases, by way of the vaginal introitus. Weakness of the pelvic ground muscles contributes to the prolapse by permitting descent of the perineum throughout straining. An necessary concept in the surgical therapy of adenocarcinoma of the rectum is the necessity of excising the rectum in continuity with the mesorectum and its contained lymph nodes so as to keep away from local tumour recurrence (Heald et al 1982). In total mesorectal excision, the posterolateral airplane of dissection is outside the mesorectal fascia however anterior to the presacral fascia and its underlying venous plexus.
Order 80 mg tadapox with visaRenal veins the renal veins are large-calibre vessels erectile dysfunction treatment natural generic tadapox 80mg otc, which lie anterior to the renal arteries and open into the inferior vena cava virtually at right angles (Ch erectile dysfunction pills sold at gnc purchase tadapox once a day. The left vein lies on the posterior stomach wall posterior to the splenic vein and body of the pancreas new erectile dysfunction drugs 2013 cheap tadapox online mastercard. It passes to the best within the angle between the abdominal aorta posteriorly and the superior mesenteric artery anteriorly erectile dysfunction recovery tadapox 80mg mastercard, to empty into the inferior vena cava. The right renal vein lies posterior to the second a part of the duodenum and, typically, the lateral part of the head of the pancreas. Lymph from the ovary can also drain via lymphatics within the broad ligament and spherical ligament to inner iliac and inguinal lymph nodes, respectively. Lymphatic drainage of the ureters is much less well outlined however follows a regional sample to nearby nodes. The lymphatic drainage of the retroperitoneal colon and rectum is described in Chapter sixty six. Whilst the medical sample of nodal metastases usually reflects normal lymphatic drainage pathways, lymphatic obstruction might lead to metastases at unusual nodal websites. Cisterna chyli and belly lymph trunks the stomach origin of the thoracic duct usually lies to the proper of the midline at the degree of the twelfth thoracic vertebral physique or the thoracolumbar intervertebral disc. It receives almost all of the lymph from below the diaphragm through the cisterna chyli, a localized lymphatic dilation fashioned mostly by the union of the intestinal lymph trunk and the left lumbar trunk (Phang et al 2014). The cisterna chyli is a saccular or fusiform lymphatic dilation measuring, on average, about 1 cm wide and a pair of cm long in the cadaver (Loukas et al 2007b). The cisterna chyli normally lies in front of the first and second lumbar vertebrae behind the best crus of the diaphragm to the right of the stomach aorta but may be positioned at the next vertebral degree. The most common configuration, present in roughly two-thirds of individuals, is a single structure formed from the union of the intestinal lymph trunk and the left (or, much less generally, the right) lumbar lymph trunk (Loukas et al 2007b). The upper two right lumbar arteries and the best lumbar azygos vein lie between the cisterna chyli and the vertebral column. The medial edge of the best crus of the diaphragm lies anterior to the belly confluence of lymph trunks. The lumbar lymph trunks are fashioned by lymphatic vessels draining para-aortic nodes. The intestinal lymph trunk (which could additionally be double) receives vessels draining from pre-aortic nodes, i. The thoracic duct leaves the superior finish of the cisterna chyli and passes through the aortic hiatus of the diaphragm posterolateral to the best aspect of the aorta. The major lymphatic vessels adjacent to the stomach aorta are at threat of damage during surgical procedures that contain peri-aortic dissection and/or lymphadenectomy. Damage to these lymphatic trunks or their obstruction by malignant disease could trigger main lymph leaks manifesting as chylous ascites or chylothorax. The brief proper suprarenal vein drains instantly into the inferior vena cava at the stage of the twelfth thoracic vertebra; the longer left vein usually joins the left renal vein and should obtain the left inferior phrenic vein. Inferior phrenic veins the inferior phrenic veins normally originate on the superior surface of the diaphragm but run mostly on its inferior floor to drain into the posterolateral aspect of the inferior vena cava. The left vein runs to the left of the oesophageal hiatus, whereas the right courses to the best of the opening in the diaphragm for the inferior vena cava, each receiving an oesophageal tributary (Loukas et al 2005b). Further, the left inferior phrenic vein incessantly communicates with the left gastric vein and hence could become prominent in portal hypertension. Both inferior phrenic veins usually drain instantly into the inferior vena cava slightly below the diaphragm, typically joining anteriorly to form a short frequent trunk. The right may often drain into the right hepatic vein or inferior vena cava above the diaphragm. In contrast, the left incessantly drains into the left suprarenal, left renal or left hepatic vein. Collaterals in inferior vena caval occlusion Obstruction of the inferior vena cava from thrombosis, embolism, extrinsic compression or intrinsic disease leads to the event of an in depth venous collateral circulation through tributaries that in the end hook up with the superior vena cava. These embody the azygos�hemiazygos venous system, the vertebral venous plexuses, and superficial physique wall veins. The midline and the level of the umbilicus kind inconstant and variable watershed boundaries for these drainage territories. Lymphatics from the deeper layers of the body wall and the abdominal and pelvic viscera drain nearly completely to the cisterna chyli and thoracic duct. The former drains by way of ipsilateral retroperitoneal lymph nodes that are concentrated around the exterior iliac and common iliac vessels and alongside the lateral features of the aorta and inferior vena cava. There is appreciable overlap between the lymphatic drainage basins of individual viscera. Some lymphatic drainage happens instantly throughout the diaphragm to the chest from the bare space of the liver. The paired retroperitoneal viscera drain to lateral aortic (also termed para-aortic) nodes around the origin of their arterial provide. Thus, the kidneys and suprarenal glands drain to nodes across the renal hilum and to lateral aortic nodes across the origin of the renal arteries (L1�2 vertebral level). The testes drain to para-aortic and paracaval nodes Retroperitoneal lymph node teams the lymphatic drainage of the rectum, colon, stomach, pancreas, oesophagus and other organs is commonly described by method of lymph node stations and levels of dissection that relate to the administration of malignant disease. The terminology and classification of retroperitoneal lymph nodes are based on their location. However, it should be noted that adjoining nodal groups merge into one another with no clear demarcating boundaries. Cross-sectional imaging incessantly makes use of 10 mm as an approximate measure for the higher limit of regular lymph node dimensions in the adult (Moeller and Reif 2000), although some normal retroperitoneal nodes, such because the portacaval node, are usually larger. Lymphatic drainage from the best testis is through lymphatics travelling with the gonadal vessels to the best para-aortic and aortocaval nodes at the stage of the second lumbar vertebra, whereas the left testis drains to the left para-aortic nodes simply inferior to the left renal vein (Pa�o et al 2011). Coeliac Abdominal confluence of lymph trunks Superior mesenteric Right lumbar lymph trunk Intestinal lymph trunk Inferior mesenteric Gonadal Suprarenal Renal Upper lateral Iliac nodes the paired iliac nodes are distributed across the widespread, exterior and inside iliac arteries and veins. Constituent teams embrace: common iliac, exterior iliac, internal iliac, circumflex iliac and obturator nodes. Obturator nodes are situated close to the obturator foramen and, together with the iliac nodes, are a common website of lymph node metastasis in prostate most cancers. The iliac nodes drain the pelvic viscera and walls, except for the ovaries and people elements of the rectum drained by superior rectal drainage pathways (see above). The first four lumbar ventral rami, along with a contribution from the twelfth thoracic ventral ramus (the dorsolumbar nerve), kind the lumbar plexus. Although there are many variations, the most typical arrangement of the plexus is described here. A branch from the ventral ramus of L1 unites with a department from the second lumbar ventral ramus to kind the genitofemoral nerve. The second, third and a lot of the fourth lumbar ventral rami divide into ventral and dorsal divisions; the ventral divisions unite to kind the obturator nerve, whereas most of the nerve fibres in the dorsal divisions kind the femoral nerve. The remaining fibres from the fourth lumbar ventral ramus be part of the fifth lumbar ventral ramus to kind the lumbosacral trunk, which descends to be a part of the sacral plexus (p. Branches from the dorsal divisions of the second and third lumbar rami unite to form the lateral femoral cutaneous nerve (lateral cutaneous nerve of thigh). The accent obturator nerve, when current, often arises from the third and fourth ventral divisions. The lumbar plexus is supplied by branches from the lumbar vessels that offer psoas major. Lateral cutaneous branches of the twelfth thoracic and first lumbar ventral rami are drawn into the gluteal pores and skin, but otherwise these nerves are just like intercostal nerves. It not solely contributes considerably to the femoral and obturator nerves, but additionally has an anterior terminal branch (the genital branch of the genitofemoral) and a lateral cutaneous branch (which contributes to the lateral femoral cutaneous nerve and the femoral branch of the genitofemoral nerve). Anterior terminal branches of the third to fifth lumbar and first sacral rami are suppressed, however the corresponding branches of the second and third sacral rami supply perineal skin. The furcal nerve is an independent nerve with its personal ventral and dorsal rootlets mostly arising alongside the L4 nerve root. Its branches contribute to the femoral and obturator nerves arising from the lumbar plexus and to the lumbosacral trunk, which joins the sacral plexus (Harshavardhana and Dabke 2014). The time period furcal refers to its forked nature because it links the lumbar and sacral plexuses. Occasionally, the furcal nerve arises at the stage of the third or the fifth lumbar nerve roots, during which case the sacral plexus is taken into account prefixed or postfixed, respectively. The cisterna chyli is more generally shaped by the intestinal lymph trunk and the left lumbar lymph trunk (rather than the proper lumbar lymph trunk shown in this diagram). Efferent lymphatics from these nodes contribute to the formation of the intestinal lymph trunk.
Order 80 mg tadapoxThe ulnar collateral ligament is normally lined by the aponeurotic insertion of the tendon of adductor pollicis erectile dysfunction pump in india cheap tadapox uk. Following avulsion erectile dysfunction with normal testosterone levels generic tadapox 80 mg overnight delivery, the proximal end can turn out to be superficially displaced around the proximal free fringe of the aponeurotic insertion of the adductor erectile dysfunction main causes buy generic tadapox 80 mg. This gentle tissue interposition prevents the ends of the avulsed ligament from therapeutic impotence ginseng effective tadapox 80 mg. Surgical repair requires division of the aponeurotic insertion of adductor pollicis, adopted by bony reattachment of the avulsed ligament and repair of the aponeurosis. The comparable damage to the radial collateral ligament is much less common and constitutes solely 10�42% of collateral ligament accidents (Edelstein et al 2008). It is attributable to sudden, forced adduction of the metacarpophalangeal joint as the outcome of a fall or throughout ball games. The ligament may be ruptured in its mid-substance or avulsed from both bony attachment. Early identification is important as a result of the proximal phalanx of the thumb will subluxate ulnarwards and should rotate, leading to degeneration of the articular surface. Interposition of the torn or avulsed portion is unusual as a outcome of the adductor aponeurosis lies over the radial collateral ligament. The patient is unable to prolong the terminal phalanx actively, although the distal interphalangeal joint could be prolonged passively. Swan neck deformity involves hyperextension of the proximal interphalangeal joint, along with distal interphalangeal joint flexion, attributable to relative overactivity of the extensors appearing on the proximal interphalangeal joint in contrast with the flexors. Boutonni�re deformity is a flexion deformity of the proximal interphalangeal joint following both division or laxity in the central slip of the extensor tendon (which normally inserts into the bottom of the center phalanx). The deformity often happens as a outcome of both trauma or rheumatoid arthritis, causing the lateral bands of the extensor tendon to migrate in a volar course and the head of the proximal phalanx to migrate dorsally. Initially, the deformity is passively correctable, but, with time, the delicate tissues around the joint contract and a onerous and fast deformity outcomes. The metacarpophalangeal joints receive their blood provide from the dorsal and palmar metacarpal arteries, the arteria princeps pollicis, and the arteria radialis indicis. The interphalangeal joints are provided by branches from the palmar digital arteries. During flexion, the cruciate fibres turn out to be oriented extra transversely within the digits, and the edges of adjoining anular pulleys approximate in order that they kind, in full flexion, a continuous tunnel of transversely oriented fibres. Surgically, crucial pulleys that prevent bowstringing of the flexor tendons are the A2 and A4 pulleys. The oblique pulley is positioned over the mid-portion of the proximal phalanx and its fibres move from the ulnar facet proximally to the radial aspect dorsally. The A2 pulley is thinner than the A1 pulley and is located just proximal to the interphalangeal joint. The oblique pulley is crucial pulley within the thumb for maintaining the motion of flexor pollicis longus. Two synovial sheaths envelop the flexor tendons as they traverse the carpal tunnel: one for flexors digitorum superficialis and profundus, the opposite for flexor pollicis longus. The sheath is extended around the tendons to the little finger and is normally continuous with their digital synovial sheath. The parietal layer strains the flexor retinaculum and the ground of the carpal tunnel, and is mirrored laterally as the visceral layer over the tendons of flexor digitorum superficialis ventrally and flexor digitorum profundus dorsally. Medially, a recess shaped by the visceral layer of the sheath insinuates between the 2 groups of tendons and passes laterally for a variable distance. The sheath of flexor pollicis longus, which is normally separate, is continued alongside the thumb so far as the insertion of the tendon. The anterior interosseous nerve and posterior interosseous nerve innervate the central two-thirds of the anterior and posterior wrist joint capsule, including the radiocarpal joint. These appear to be pure afferent nerve fibres with mechanoreceptor endings, of which there are a median of 10 in every dorsal radiocarpal ligament (Tomita et al 2007). In the palmar radiocarpal ligaments, nevertheless, Golgi organs, Pacinian corpuscles, Ruffini endings and free nerve endings are discovered (Petrie et al 1997). An uneven distribution of these all through the ligaments would suggest particular practical adaptation however the exact nature of this is unclear. The carpometacarpal joint of the thumb is innervated by articular twigs from the posterior interosseous nerve and the superficial department of the radial nerve. The second to fifth carpometacarpal joints are innervated by branches of the ulnar nerve, the anterior interosseous, and the superficial radial and dorsal ulnar nerves. The metacarpophalangeal joints are innervated by twigs from the palmar digital branches of the median and ulnar nerve, the deep terminal branch of the ulnar nerve, and the posterior interosseous nerve. The interphalangeal joints are innervated by the palmar digital branches of the median nerve (to the thumb, index, center and ring fingers), and the ulnar nerve (to the ring and little fingers). Vincula Flexor tendon sheaths the fibrous sheaths of the flexor tendons are specialized parts of the palmar fascia. Each finger has an osseo-aponeurotic tunnel that extends from midpalm to the distal phalanx. The thumb has a tunnel for flexor pollicis longus that extends from the metacarpal to the distal phalanx. The proximal border is, to some extent, a matter of definition as a result of the transverse fibres of the palmar aponeurosis may be thought of to be a half of the pulley system. The sheath consists of arcuate fibres that arch anteriorly over bone, tendons (where the sheath is required to be stiff) and the centres of joints (where a bucket-handle of arcuate fibres is a mechanically favourable arrangement). In contrast, where the sheath is required to fold to permit joint flexion, it consists of cruciate fibres. These fibrous sheaths are lined by a thin synovial membrane that gives a sealed lubrication system containing synovial fluid. The sheaths around the thumb and little finger are continuous with the flexor sheaths in entrance of the wrist. The parietal synovial membrane is mirrored on to the floor of the flexor tendon, forming a visceral synovium. A commonplace nomenclature for the anular (A) and cruciform (C) pulleys is used (Doyle and Blythe 1975). The A1 pulley is located anterior to the palmar cartilaginous plate of the metacarpophalangeal joint and should lengthen over the proximal part of the proximal phalanx. It is the strongest pulley and arises from well-defined longitudinal ridges on the palmar side of the phalanx. A pouch or recess of synovium extends superficial to the free fringe of the pulley fibres so that the free edge forms a lip protruding into the synovial space. A4 overlies the center third of the center phalanx, and A5 overlies the distal interphalangeal joint. The tendons of abductor pollicis longus and extensor pollicis brevis lie in a tunnel on the lateral facet of the styloid process of the radius; there could additionally be a separate synovial sheath for every, or the tendon of the abductor may be double. The tendons of extensors carpi radiales longus and brevis lie behind the styloid process; the tendon of extensor pollicis longus lies on the medial side of the dorsal tubercle of the radius; the tendons of extensors digitorum and indicis lie in a tunnel on the medial aspect of the tubercle; the tendon of extensor digiti minimi lies reverse the interval between the radius and ulna; and the tendon of extensor carpi ulnaris lies between the pinnacle and the styloid means of the ulna. The tendon sheaths of abductor pollicis longus, extensors pollicis brevis and longus, extensors carpi radiales and extensor carpi ulnaris cease instantly proximal to the bases of the metacarpal bones, while those of extensors digitorum, indicis and digiti minimi are typically prolonged somewhat extra distally alongside the metacarpus. Folds of synovial membrane containing a loose plexus of fascial fibres carry blood vessels to the tendons at certain outlined factors. Vincula brevia, of which there are two in every finger, are connected to the deep surfaces of the tendons close to to their insertions. There is, thus, one vinculum brevium attaching flexor digitorum profundus to the region of the distal interphalangeal joint, and a more proximal vinculum deep to flexor digitorum superficialis at the proximal interphalangeal joint. Vincula longa are filiform; usually two are connected to every superficial tendon, one to every deep tendon. The affected sheath thickens and entraps the contained tendons, which become constricted on the web site of entrapment and bulge distal to it. This produces a definite nodule in the palm of the hand and the finger now snaps as the tendon nodule passes by way of the constriction on flexing the finger. The corresponding extensor muscle is insufficiently powerful to prolong the affected finger, so the patient does this passively, accompanied by a painful snap. Treatment frequently requires surgical division of the A1 pulley of the flexor sheath to relieve the stricture. It entails the widespread extensor sheath containing the tendons of abductor pollicis longus and extensor pollicis brevis. There is palpable thickening of the tendon sheath with painful limitation of extension of the thumb. Treatment frequently requires division of the thickened sheath, care being taken to avoid the adjoining superficial radial nerve; division of the sheath produces no functional impairment.
|
|

