|
"Differin 15 gr generic overnight delivery, acne bacteria". J. Delazar, M.B. B.A.O., M.B.B.Ch., Ph.D. Medical Instructor, New York Institute of Technology College of Osteopathic Medicine at Arkansas State University
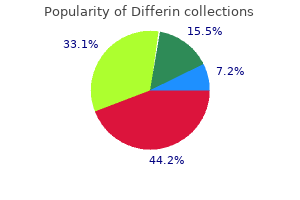
For the needs of this chapter, "structural heart disease" encompasses primary anatomic cardiac abnormalities similar to congenital coronary heart disease, valvar stenosis and/or regurgitation unbiased of a congenital abnormality, and coronary artery disease. This is in distinction to cardiomyopathies and pericardial disease, which primarily have an result on cardiac muscle and the pericardium, respectively. Broadly speaking, from the standpoint of age, youngsters could be divided into two broad teams: neonates/infants (<1 yr of age) and children/adolescents; the etiologies of chronic coronary heart failure in these populations are likely to be distinct, although overlap certainly exists. Neonates and Infants the neonate or infant with coronary heart failure sometimes presents for care after an episode of acute sickness during which the diagnosis of coronary heart failure is made, hemodynamic instability and symptoms are stabilized, and medical management is initiated. In some instances, the prognosis is evident, though in a considerable proportion of cases, the diagnosis remains unclear and the kid is left with the analysis of "idiopathic dilated cardiomyopathy. The Ross classification for coronary heart failure in youngsters after 25 years: a review and an age-stratified revision. Broadly talking, potential etiologies of continual coronary heart failure in neonates and infants can be grouped underneath infectious, inflammatory, toxic, structural/congenital, metabolic, arrhythmogenic, and idiopathic. The differential diagnosis for the unusual presentation of heart failure at the time of birth includes delivery asphyxia with myocardial dysfunction from hypoxemia, hypoglycemia, hypocalcemia, sepsis, anemia or polycythemia, myocarditis, arrhythmias (congenital complete coronary heart block, supraventricular tachyarrhythmias), giant arteriovenous malformations, extreme atrioventricular valve regurgitation, or Ebstein abnormality of the tricuspid valve (13). Essentially any type of congenital coronary heart disease can precipitate ventricular dysfunction, although ventricular dysfunction with resultant symptoms of low cardiac output are typically restricted to the following physiologic derangements: (a) obstructive lesions. Without upkeep of ductal patency with prostaglandin E1, affected infants usually present within the first 1 to 2 weeks of life with signs and symptoms of low cardiac output, together with but not restricted to pallor, poor feeding, weak cry, acidosis, shock, and ranging degrees of cyanosis due to intracardiac mixing. The creation of pulse oximetry screening has made it possible to identify readily infants with ductal-dependent cyanotic congenital heart illness who could otherwise escape detection earlier than discharge from the new child nursery (14); the effects on infant outcomes of a nationwide implementation of this apply remain unclear, but no less than seem to be cost efficient (15,16,17). The clinical presentation of quantity overload lesions relies upon upon the dimensions of the defect and the ratio of pulmonary to systemic vascular resistance. During the neonatal interval, the ratio may be practically equal, resulting in a well-balanced circulation and little internet left-to-right shunt. However, as pulmonary vascular resistance falls usually with age, the proportion of pulmonary blood circulate increases, with a lower in the ratio of systemic blood move. This progressive internet left-to-right shunt may result in impaired cardiac output (18), which may be accentuated by periods of increased metabolic demand (fever) or by the physiologic fall in hemoglobin (19). The prototypic regurgitant lesion inflicting symptoms of a low cardiac output and heart failure in the neonate and/or infant is Ebstein anomaly of the tricuspid valve. The anatomy and physiology of this lesion is described intimately in Chapter 38 of this textbook. When severe, the mixture of significant tricuspid regurgitation and practical right ventricular hypoplasia leads to a state in which the proper ventricle is unable to generate adequate forward output. Frequently, nonetheless, the pulmonary valve in Ebstein abnormality is incompetent, leading to an inefficient cycle in which deoxygenated blood is recirculated through the heart, resulting in worsening cyanosis even within the setting of ductal patency (20). This units off a vicious cycle, generally termed a "circular shunt," in which cyanosis and low cardiac output are intertwined. Many advanced congenital abnormalities are associated with each obstruction and volume overload, which can lead to a combination of heart failure and cyanosis. Patients with single ventricle physiology, will incessantly fall into this category. The particular manifestations of heart failure and cyanosis, and their severity, rely upon the balance of systemic and pulmonary vascular resistance in addition to the precise anatomic traits of the defect. As an instance, in tricuspid atresia with usually associated great vessels, a large muscular ventricular septal defect, and no pulmonary stenosis, the patient may require no interventions as a neonate but finally require a further source of pulmonary blood move later in infancy due to progressive cyanosis as a result of the development of restriction at the ventricular septal defect. The quite a few categories and variations of the advanced defects capable of causing both strain and volume overload are mentioned in detail of their respective chapters. The anatomy, physiology, and treatment of this lesion are described in detail in Chapter 32. Its clinical presentation depends upon the traditional fall in pulmonary vascular resistance; as pulmonary vascular resistance and pressure fall, perfusion pressure within the left coronary artery falls in concert. This leads to the gradual development of myocardial ischemia within the areas provided by the left coronary artery, with signs sometimes turning into manifest between 1 week and 6 months of age. Recognition of this defect because the underlying reason for ventricular dysfunction is of paramount significance as a outcome of the ensuing heart failure syndrome may be largely reversed by prompt surgical revascularization of the ischemic myocardium supplied by the traditional left coronary artery distribution (23,24,25). Misguided attempts at prolonged medical administration may worsen the underlying physiology, lose necessary time in rescuing ischemic myocardium, and in the end provide no long-term profit to the affected person. Myocarditis and all the varied cardiomyopathies (dilated, hypertrophic, restrictive, noncompaction, arrhythmogenic proper ventricular dysplasia, tachycardia-induced) might current in the course of the neonatal interval or infancy with signs of coronary heart failure, sometimes instantly related to ventricular dysfunction. Following hemodynamic stabilization, treatment and prognosis are regularly directed by the underlying diagnosis. In neonates and infants, a low index of suspicion ought to be maintained for cardiomyopathies associated with inborn errors of metabolism, together with mitochondrial illness, till session with an expert in metabolic problems is obtained (26,27,28). Some practitioners advocate empiric carnitine supplementation for all suspected metabolic cardiomyopathies, or a minimum of till the prognosis of carnitine deficiency is excluded, although the benefits of those practices are questionable (29). It is useful to subdivide heart failure in this age group into left versus right heart failure. Left coronary heart failure might occur in sufferers with structural coronary heart disease and severe atrioventricular valve insufficiency. Although progression of valvar regurgitation may occur spontaneously over time, infective endocarditis is an important etiology of altered valvar perform on this group of patients (36). Less commonly, patients with either progressive or undiagnosed severe left ventricular outflow tract obstruction might current with heart failure due to ventricular dysfunction (37). An necessary cause of right coronary heart failure in this group of sufferers is Ebstein anomaly of the tricuspid valve with an increase within the degree of tricuspid regurgitation with or without related arrhythmias (38,39). Severe elevation of pulmonary vascular resistance related to an intracardiac shunt or nice vessel shunt P. Postoperative Structural Heart Disease More common is the patient who has undergone earlier intervention (transcatheter or surgical) for structural heart disease. Such sufferers could develop left or right coronary heart failure because of ventricular dysfunction, valve illness, residual shunts, and/or rhythm abnormalities (32,42). Examples embody (a) aortic valve stenosis and/or insufficiency after earlier surgical valvotomy (43,44,45) or balloon valvuloplasty (46,forty seven,48), (b) truncal valve stenosis and/or regurgitation after restore (45,49,50,51), and (c) extreme atrioventricular valve regurgitation after atrioventricular septal defect repair (52,fifty three,54). Right ventricular hypertension owing to pulmonary hypertension (65) or residual pulmonary outflow tract obstruction (native or conduit) (66,sixty seven,68) might progress after initial intervention and end in proper coronary heart failure. Right heart failure may happen after earlier intervention owing to significant pulmonary insufficiency, similar to could happen after surgical procedure for tetralogy of Fallot (69,70,71). A promising new therapy in the treatment of residual proper ventricular outflow tract disease is transcatheter pulmonary valve alternative, which permits a less invasive methodology of restoring pulmonary valve competence and decreasing obstruction with out exposing the patient to cardiopulmonary bypass (72,73,74). The long-term effects of this new treatment option on the evolution of proper heart dysfunction in tetralogy of Fallot and related lesions remain to be seen. Heart transplantation might supply the best alternative for long-term survival in the inhabitants of Fontan sufferers in whom coronary heart failure develops, as they regularly reply poorly to conventional medical and gadget therapy for heart failure. However, they seem to have poorer posttransplantation outcomes than patients without pre-existing Fontan physiology or congenital coronary heart illness (79). As said previously, sufferers after transcatheter or surgical intervention for structural heart illness might develop both acute or persistent rhythm disturbances that will end in coronary heart failure (77,80,81,82). Ventricular dyssynchrony, manifested by conduction delay on the electrocardiogram, may contribute to symptomatic ventricular dysfunction. Efforts to restore ventricular electrical and mechanical ventricular synchrony by way of biventricular pacing are described later in this chapter. Structurally Normal Heart and Acquired Heart Disease In growing nations, rheumatic heart disease is the most typical explanation for acquired heart illness in kids and younger adults, manifesting as carditis in the acute section of illness (83,84). Acute rheumatic fever is uncommon in the United States, although intermittent outbreaks of the illness continue to happen in clusters (85). Acute insufficiency of one or either of these valves could lead to acute ventricular dilation and symptoms of heart failure from acute changes in ventricular loading situations in 15% to 47% of sufferers (89,ninety,91). Valvar stenosis and/or insufficiency develops with continual rheumatic coronary heart illness, with a low incidence of involvement of the tricuspid and/or pulmonary valves (92). Less commonly, left ventricular dysfunction may develop secondary to persistent severe volume overload if significant mitral and/or aortic regurgitation are current. Although rheumatic mitral stenosis severe sufficient to end in symptomatic heart failure could occur within the first two decades of life in developing international locations (95), chronic rheumatic heart disease with mitral stenosis within the United States usually presents in the fourth to fifth decade of life (83). Kawasaki illness is a vital cause of acquired heart illness in developed countries and is the most typical cause of acquired coronary heart illness in children within the United States (96). Children lower than 5 years are most commonly affected, with a median age of 2 years at prognosis. Another hallmark characteristic of Kawasaki disease is that almost all affected people develop a pancarditis, which may manifest with echocardiographic proof of ventricular dysfunction and/or symptomatic coronary heart failure (99). Infective endocarditis may cause heart failure in older kids with structurally regular hearts, although the incidence of endocarditis is considerably lower than that observed in sufferers with unrepaired or palliated congenital coronary heart illness with residual intracardiac shunts, who symbolize the best danger for endocarditis (103,104).
Additional information:
Moreover, false tendons and bands in the apical portion of the left ventricle are normal findings that would result in overdiagnosis. Although there stays some competition as to the precise standards to fulfil the prognosis, Jenni et al. Solid arrows represent noncompact: compact ratio and broken arrows symbolize trabeculations. Our conclusion is that Jenni standards endure the most acceptable normal if it is adopted appropriately (10). Inclusion or exclusion of the trabeculations within the measurement remains contentious as discussed previously. The transmitral inflow pattern sometimes demonstrates a restrictive filling sample with an elevated P. Tissue Doppler velocities typically show a discount in Ea, Aa, and Sa velocities (137). Absence of cardiac anomalies >3 distinguished trabeculae visible in one image airplane at finish diastole that moves synchronously with the compacted myocardium. Left ventricular noncompaction: a genetic cardiomyopathy looking for diagnostic standards. Some of the cardiac segments with noncompacted areas might be evaluated utilizing speckle tracking imaging for longitudinal pressure. Although the majority of sufferers have noncompaction isolated to the left ventricle, biventricular involvement has been properly documented (Video 54. Finally to keep away from the overdiagnosis of this entity, using distinction echocardiography could show very helpful (173,174). This could also be significantly true in older adolescent patients, overweight sufferers, or patients supported on mechanical air flow. Contrast echocardiography may outline prominent false tendineae or apical bands. Better border definition and improved visualization of the apex might enhance measurement accuracy in these regions (Videos fifty four. Delayed contrast hyperenhancement can be utilized to assess perfusion defects and the presence of myocardial fibrosis (187,188,189,one hundred ninety,191,192). Patients with regular ejection fraction may require no medical therapy or simply aspirin remedy. Hypertrophic cardiomyopathy phenotype may warrant -blocker or calcium channel blocker remedy. Many patients are handled with antiplatelet agent such as aspirin to forestall in opposition to thromboembolic events that outcome from thrombi that develop within the crypts. Patients with confirmed metabolic illness may be treated with a mixture of carnitine, coenzyme Q, and riboflavin/thiamine (7). Collaboration and multidisciplinary assessment with a specialist in metabolic illness is extremely recommended in this circumstance. Some sufferers will fail medical therapy and demonstrate multisystem organ failure requiring cardiac transplantation. These sufferers might require long-term support with intravenous inotropes or even mechanical assist as a bridge to transplantation. Some patients with univentricular circulation have even had palliation to complete cavopulmonary communication (198). Some authors have advocated that coronary insufficiency may contribute to the hypertrabecular appearance of the myocardium (205). Reimold described de novo left ventricular trabeculations creating during being pregnant in several girls that later regressed (206). Deconditioning and reexamination with echocardiography or another imaging modality is beneficial before diagnosing the condition on this setting. Many adult patients could only present in later maturity highlighting a benign course all through their early years (214,215). Given that completely different gene mutations result in various phenotypes, this info might not present definitive prognostic data. It is also likely that epigenetic elements affect specific gene mutations in the clinical phenotype of the disease (6,217). The etiology varies from idiopathic to particular gene mutations to metabolic problems. The lack of uniform constant standards in analysis could also be responsible for under- and overdiagnosis of the condition in different settings. Although the future for research on this fascinating condition is promising, a unified reproducible imaging and diagnostic coverage is important to dispel confusion about this disease entity. The following are some areas where common settlement can be beneficial and illuminating: A. This is necessary as one might erroneously diagnose a critical condition with work and insurance implications. Trabeculations may progress over time and will change beneath different physiologic circumstances corresponding to being pregnant. Athletes could manifest options of hypertrabeculation which are physiologic responses just like athletic heart. Screening first-degree family members, particularly siblings and parents, is crucially important given the reported familial cases. Future developments similar to cardiac resynchronization therapy might circumvent the necessity for orthotopic coronary heart transplantation in patients who fail medical remedy (218). Left ventricular noncompaction revisited: a distinct phenotype with genetic heterogeneity Left ventricular noncompaction and cardiomyopathy: cause, contributor, or epiphenomenon. Report of the 1995 World Health Organization/International Society and Federation of Cardiology. Echocardiographic and pathoanatomical traits of isolated left ventricular non-compaction: a step in direction of classification as a distinct cardiomyopathy. Congenital heart illness with a quantity of cardiac anomalies: report of a case displaying aortic atresia, fibrous scar in myocardium and embryonal sinusoidal remains. The nature of the vascular communications between the coronary arteries and the chambers of the heart. Anomalous cardiac blood vessel communicating with the proper ventricle; observations in a case of pulmonary atresia with an intact ventricular septum. Embryonal sinusoids within the myocardium: report of a case efficiently handled surgically. Identification of a uncommon congenital anomaly of the myocardium by two-dimensional echocardiography: persistence of isolated myocardial sinusoids. Anomalous ventricular myocardial patterns in a baby with complicated congenital heart illness. Isolated left ventricular non-compaction: an unclassified cardiomyopathy with severe prognosis in adults. Left ventricular noncompaction: a distinct cardiomyopathy or a trait shared by different cardiac illnesses Peripartum cardiomyopathy related to left ventricular noncompaction phenotype and reversible body rotation. Reversible de novo left ventricular trabeculations in pregnant girls: implications for the diagnosis of left ventricular noncompaction in low-risk populations. Heuristic issues in defining the three-dimensional association of the ventricular myocytes. P57Kip2 expression is enhanced during mid-cardiac murine improvement and is restricted to trabecular myocardium. Abberant neural and cardiac improvement in mice missing the ErbB4 neuregulin receptor. Nkx2�5 pathways and congenital coronary heart disease; lack of ventricular myocyte lineage specification results in progressive cardiomyopathy and complete coronary heart block. A heart segmental defect within the anterior-posterior axis of a transgenic mutant mouse. Hypoxia-inducible transcription factor-1alpha triggers an autocrine survival pathway throughout embryonic cardiac outflow tract remodeling. Convergent proliferative response and divergent morphogenic pathways induced by epicardial and endocardial signaling in fetal heart development. Activation of Notch1 signaling in cardiogenic mesoderm induces irregular coronary heart morphogenesis in mouse. Monitoring Notch1 activity in improvement: proof for a feedback regulatory loop. Tbx20 a downstream mediator for bone morphogenetic protein 10 in regulating cardiac ventricular wall improvement and performance.
Cardiac resynchronization therapy for pediatric patients with coronary heart failure and congenital heart illness: a reappraisal of outcomes. Classic-pattern dyssynchrony and electrical activation delays in pediatric dilated cardiomyopathy. Left ventricular help device in Duchenne cardiomyopathy: Can we modify the pure historical past of cardiac disease Long-term outcomes of dilated cardiomyopathy diagnosed during childhood: outcomes from a national population-based study of childhood cardiomyopathy. Competing dangers for dying and cardiac transplantation in youngsters with dilated cardiomyopathy: results from the pediatric cardiomyopathy registry. New mechanistic and therapeutic targets for pediatric heart failure: report from a National Heart, Lung, and Blood Institute working group. Newburger the survival of kids with congenital coronary heart illness has improved dramatically over the past 4 decades. As a outcome, the variety of adults with congenital heart illness is now believed to exceed the number of children (1,2,three,4). Poor faculty performance and the resultant need for academic help throughout the developmental span from kindergarten through 12th grade may have considerable personal and societal costs. Furthermore, the rising variety of adults with congenital heart illness has highlighted the consequences of neurodevelopmental impairments for employability and psychological well being (5). Neurodevelopmental disabilities can derive from innate or genetic elements, from aberrant fetal circulation, from the physiology and sequelae of congenital heart illness itself. Particularly in congenital coronary heart disease, it can be troublesome to separate developmental outcomes for a selected prognosis and its genetic underpinnings from penalties of surgical and transcatheter procedures utilized in its administration. It is probably going that central nervous system results of congenital heart disease are cumulative and affected by the complicated interplay of genetic, preoperative, intraoperative, and postoperative elements (6,7). In this chapter, we evaluate variables that contribute to neurodevelopmental outcomes in children after coronary heart surgery and summarize findings associated to long-term neurodevelopmental outcomes for extra frequent, complicated congenital coronary heart malformations. Genetic Abnormalities Genetic abnormalities could cause each congenital heart defects and abnormalities of central nervous system structure and performance. Children with genetic syndromes have a lot worse neurodevelopmental consequence than those without recognizable syndromes (8,9). For example, though the clinical phenotype associated with 22q11 microdeletion is variable (18), a reasonably constant neurodevelopmental profile has emerged. In adults with velocardiofacial syndrome, specific deficits have been reported in visual� spatial ability, downside solving and planning (executive functions), abstract social considering, and attentiveness (23,25,26). Finally, some genetic mutations that cause structural heart defects are associated with psychiatric sickness, including, the 22q11 microdeletion (19,23,28,29,30,31,32). In adults with 22q11 microdeletion, the prevalence of late-onset psychosis, mostly schizophrenia and schizo-affective issues, is 10% to 20% (21,33,34). Brain Anatomy, Pathology, and Neuroimaging Cerebral dysgenesis has been reported in autopsy series to occur in 10% to 29% of kids with congenital heart disease and will include such features as microdysgenesis, incomplete operculization, microcephaly, and agenesis of the corpus callosum (7,35,36,37,38). The reason for cerebral dysgenesis could also be associated to genetic elements or to abnormalities of fetal cerebrovascular hemodynamics attributable to the actual congenital coronary heart defect. Fetuses with congenital heart illness and with low cerebral-to-placental resistance ratios (<1) have smaller head circumferences than normal (41). Multiple research have demonstrated an association of smaller brains and congenital coronary heart illness (41,43,forty four,45). Thromboembolic occasions associated to cardiac catheterization, cardiac surgical procedure, or endocarditis could cause focal infarction. Decreased cerebral perfusion, related to hypotension, hypoperfusion, or cardiac arrest, is related to a diffuse pattern of cerebral harm (46). Neonates had been extra doubtless than infants to have periventricular leukoencephalopathy, reflecting the vulnerability of the immature (premyelinating) white matter to hypoxic�ischemic harm. Otherwise, the timing and sort of surgery had been unrelated to the sample and severity of general mind harm. The Total Maturation Scoring System developed by Childs to measure brain maturation in untimely infants incorporates info associated to myelination, cortical infolding, glial cell migration bands, and the presence of germinal matrix tissue (49). In the early postoperative period, 48% of infants had new periventricular leukoencephalopathy, 19% had new infarcts, and 33% had new parenchymal hemorrhage. Changes in central nervous system construction may underlie neurocognitive abnormalities in youngsters with congenital heart disease. For example, worse performance in math downside solving and numerical operations was correlated with decreased left parietal fractional anisotropy. In a blended group of congenital coronary heart illness adolescents, compared to controls, mind volume was reduced, and the extent of mind volume reduction was considerably related to scores on tests of cognition, executive perform, and motor operate (56). Perioperative Risk Factors Prospective research of central nervous system protection and harm have primarily centered on risk components associated to cardiac surgical procedure and the perioperative interval. The intense attention to perioperative danger factors is in all probability going associated to the ability of investigators to research the mind during this high-risk period, which incorporates deliberate brain ischemia�reperfusion harm with use of hypothermic cardiopulmonary bypass and complete circulatory arrest techniques. Perioperative Monitoring Approaches As investigators have sought to optimize neurodevelopmental outcomes by modifying surgical and medical perioperative approaches, one limiting factor has been problem in identifying early predictive markers of longerterm developmental outcomes. However, some centers have adopted perioperative monitoring strategies that embody steady electroencephalogram, nearinfrared spectroscopy, and/or transcranial Doppler ultrasound (51,fifty seven,58). Clinical adoption of these monitoring strategies has outpaced establishment of definitive evidence for their scientific profit. Further examine of this technique, different perioperative monitoring approaches and additional potential early markers are wanted to higher perceive how late outcomes can be predicted in newborns and infants undergoing cardiac surgical procedure. Nonetheless, a great deal has been discovered because the Nineteen Nineties associated to perioperative threat factors of central nervous system insults for children with congenital heart disease. Intraoperative Support Techniques Repair of congenital coronary heart disease commonly requires the usage of cardiopulmonary bypass, during which blood is uncovered to artificial surfaces. Furthermore, cardiopulmonary bypass is accompanied by risks of gaseous and particulate embolism, macroemboli, and hypoperfusion leading to diffuse ischemia/reperfusion harm (61). Its effects are derived, partly, from a discount in metabolic activity reflected in decreased oxygen consumption. Additional mechanisms of hypothermic protection of the brain and other organs during ischemia include preservation of intracellular stores of high-energy phosphates and of high intracellular pH, as properly as protection towards reperfusion damage together with the no-reflow phenomenon, calcium inflow, and free radical damage (65). Circulatory arrest has been widely used since the 1960s in centers with experience in toddler open cardiac surgical procedure. This approach has benefits for the surgeon of absence of perfusion cannulae and of blood from the operative subject, although it may increase the risk for neurologic insult. When evaluated as a steady variable, an extended duration of complete circulatory arrest has been related to increased threat of seizures, choreoathetosis, release of brain isoenzymes, and developmental delay (71,72,seventy three,seventy four,seventy five,76,seventy seven,seventy eight,79,eighty,81) though in some research, the period of circulatory arrest has not been a significant predictor of outcome (68,82). The absence of an impact could also be related, in part, to a slim range of circulatory arrest instances, small pattern sizes, or overwhelming effects of different threat elements for adverse end result, corresponding to underlying genetic abnormalities or extreme hemodynamic instability within the preoperative or postoperative interval. Hemodilution throughout hypothermic cardiopulmonary bypass has also been studied with respect to its effects on mind harm throughout toddler heart surgery. At the profoundly low temperatures (15� to 18�C) used during toddler and neonatal cardiac surgery, hypothermia will increase the viscosity of blood and purple blood cell aggregation (91), potentially increasing the risk of microvascular occlusion. Hemodilution has been used to counter these dangers (92) and has been shown to increase cerebral blood circulate (93), however might cut back the oxygen-carrying capacity of blood. Furthermore, as a outcome of hypothermia induces a leftward shift of oxyhemoglobin dissociation, hemodilution has the potential to restrict oxygen supply to the central nervous system (92). A subsequent trial confirmed no variations in neurodevelopmental outcome at 1 12 months with hemodilution inside the vary of 25% to 35% (94). It is probably going that components similar to hematocrit, temperature, pH strategy, and duration of circulatory arrest or very reduced flow work together in their effects on the central nervous system (95,96). For instance, the reduced oxygencarrying capability of a low hematocrit throughout cardiopulmonary bypass could be compensated for by means of the pH-stat technique, by rising move rate, reducing the length of circulatory arrest, or decreasing temperature. Preoperative Factors and Host Susceptibility Host susceptibility is prone to have an result on the response of the central nervous system to cardiopulmonary bypass and perioperative events (97). Preoperative affected person characteristics corresponding to low Apgar scores at 5 minutes, youthful gestational age, decrease start weight, and different attributes have been found to be unbiased risk elements for opposed neurodevelopmental outcomes (89,98). Furthermore, the response to cardiac surgery may be mediated by genetic polymorphisms in the pathways affected by exposure to cardiopulmonary bypass, together with irritation, thrombosis, vascular reactivity, and oxidative stress (100). The influence of genetic polymorphisms on postoperative morbidity has been extensively studied among adults undergoing open heart surgical procedure (101,102,103,104,105). For example, postoperative bleeding is extra common amongst adults with polymorphisms in genes coding for coagulation proteins and platelet glycoproteins (105), whereas postoperative thrombotic issues have been associated with gene polymorphisms in fibrinogen and angiotensin-converting enzyme (106). Interestingly, this discovering underscores that youngsters and adults may differ with respect to the effects of specific genotypes. Postoperative Factors Various threat components for brain damage occur within the postoperative period. A low cardiac output syndrome is frequent in the first 24 to 48 hours following restore of complex congenital coronary heart disease (115,116).
Preoperative (prior to an arterial swap operation) stroke has been discovered by some to be associated with balloon atrial septostomy (74), nevertheless this finding has been refuted by others (75) and is felt somewhat to be due to oxygenation and time to surgical procedure. Regardless, balloon atrial septostomy is a key and important component in the care of infants with transposition of the great arteries. Other Interventional Procedures A variety of interventions within the cardiac catheterization laboratory could need to be carried out in follow-up of patients after surgical restore. Patients with Senning and Mustard operations might have baffle leaks (often resulting in desaturation) that may be closed in the cardiac catheterization laboratory with gadgets or lined stents (76,seventy seven,78). While some have advocated for a "hybrid" (combined interventional and surgical approach) to deal with pulmonary venous obstruction (80), in our experience, percutaneous stent remedy is possible despite the acute angle catheter course to the pulmonary venous atrium. Narrowing of the pulmonary venous baffle is seen (arrows) on the anterior�posterior (with cranial angulation) (A) and lateral (B) projections. The outcomes of balloon dilation are blended on this setting and may be more favorable if a discrete space of narrowing is current. Stent remedy in this area may lead to creation of an iatrogenic aortopulmonary artery window due to the close proximity of the neo primary pulmonary artery with the aorta in the absence of a tissue plane. A further consideration of stent placement in this setting is both stent fracture (83) or distortion of the neo-aortic sinuses and resultant neo-aortic regurgitation, in patients in whom the relationship of the 2 great vessels is in close proximity. The possibility of compression of the coronary arteries must also be dominated out previous to stent placement in the main pulmonary artery. Pulmonary branch angioplasty/stent placement could also be indicated in patients following an arterial switch operation. Due to related reasons, formation of an iatrogenic aortopulmonary window might occur after balloon angioplasty or stent placement in P. Importantly, interventional cardiac catheterization with balloon angioplasty and/or stent placement may be indicated for sufferers with necessary coronary artery lesions after an arterial change operation (86). Proximity to the coronary arteries should be examined prior to stent placement/percutaneous valve placements in these conduits. Most residual ventricular septal defects after a Rastelli operation may also be closed percutaneously in the cardiac catheterization laboratory. Operative Procedures Transposition of the great arteries is primarily a surgical disease. Early within the surgical expertise, correction was directed at atrial stage redirection procedures (Senning. These provided a physiologic correction however left the right ventricle and tricuspid valve within the systemic circulation with the potential for long-term adverse sequelae together with proper ventricular dysfunction, tricuspid regurgitation, and a high incidence of arrhythmias. Although attempts at anatomic correction of transposition at the arterial degree predated the Senning and Mustard procedures, there have been no survivors of these early attempts (88), and physiologic correction/atrial degree procedures grew to become the usual of care. The main technical difficulty for anatomic correction at that time was the coronary transfer. As experience was gained with aortocoronary bypass and microvascular surgical techniques, arterial level switches together with switch of the coronary arteries turned possible. In 1975, Jatene carried out the first successful arterial swap process with translocation of the coronary arteries to the neo-aortic root in a 40-day-old toddler with transposition and ventricular septal defect (3). This operation is considered by some to be "one of many biggest contributions in pediatric cardiac surgical procedure of latest times. This operation represents a monumental contribution to the therapy of congenital heart disease. Although the next five patients died earlier than his next profitable arterial change operation, Jatene had demonstrated that this technique was possible and would enable for an anatomic correction of this lesion. As expertise accrued and postoperative care improved, operative mortality rapidly declined and currently survival for the arterial change operation approaches one hundred pc in skilled facilities (56,57,58,59,60). Because of the poor results with atrial stage procedures in sufferers with transposition and ventricular septal defect, the long-term issues with proper ventricular dysfunction, tricuspid valve regurgitation, and the long-term morbidity, particularly with arrhythmias within the atrial degree switch, and with the wonderful results achieved with anatomic correction, the arterial change operation. In these patients with transposition with ventricular septal defect and left ventricular outflow tract obstruction, the arterial change operation stays the procedure of choice if the outflow tract obstruction could be surgically addressed. Long-Term Outcomes and Young Adult Issues Although the short-term effects of cyanosis have been mitigated with atrial redirection procedures, for instance, the Mustard and Senning operations, these circulations in the long run are fraught with the issue of leaving the morphologic right ventricle as the systemic ventricle, together with other sequelae. In a big cohort of 339 patients from six hospitals in Belgium (90), actuarial survival of early survivors of the Senning and Mustard operations was 91. Atrial arrhythmias are widespread in patients having undergone atrial redirection procedures (between 5% and 29%) (79). Late age at initial repair and presence of a ventricular septal defect additionally probably influence the development of pulmonary hypertension. If the pulmonary vascular resistance is too high or not reactive, heart�lung transplantation or heart transplantation with a postoperative proper ventricular help system may be wanted. Takedown of Senning and Mustard circulations, after pulmonary artery band placement to "put together" the morphologic left ventricle was traditionally carried out (70,71,ninety two,93), with success in most sufferers. It is unlikely that a morphologic left ventricle could be efficiently retrained after the age of 12 (71). The uncommon exception to this is in a position to be a patient with transposition of the great arteries ventricular septal defect and left ventricular outflow tract obstruction who presents late, whose left P. However, in lots of of these sufferers, a dilated systemic proper ventricle leads to an unfavorable configuration for a systemic ventricle. The aorta could be seen anterior and originating from the systemic proper ventricle with the pulmonary artery being posterior and originating from the left ventricle. Large research from skilled centers have reported actuarial survival of 96% at 7 years. Lifelong follow-up is important in these sufferers for monitoring for supravalvar neo-pulmonary stenosis, branch pulmonary artery stenosis, semilunar valve operate, neo-aortic root dilation. Long-term follow-up research thus far present that neo-aortic regurgitation is widespread in these sufferers (mild-22% to 26%, reasonable or more-1% to 9%), however neo-aortic valve restore or replacement is unusual (94,95). Neo-pulmonary valve regurgitation can similarly be seen, although hardly ever needs to be addressed in the expertise so far. Practitioners ought to have a low threshold for suspicion of coronary events in follow-up after the arterial switch operation. In a large study from France, coronary occasion free survival was 88% at 15 years (40). Treatment could also be needed in the cardiac catheterization laboratory or operating room (40,86). Historical long-term follow-up for sufferers having undergone the Rastelli operation show transplantation-free survival in two massive sequence found to be in the range of 52% to 58% at 20 years (97,98). Reoperation for proper and left ventricular outflow tract obstruction is common with 21% freedom from reintervention for proper ventricular outflow tract obstruction at 15 years (97) and 33% at 20 years (98). Freedom from reintervention for left ventricular outflow tract obstruction in the identical two sequence was 84% at 15 years (97) and 93% at 20 years (98). Due to aggressive resection of the left ventricular outflow tract obstruction substrate, in their expertise, recurrent left ventricular outflow tract obstruction was uncommon (5% chance throughout 25-year follow-up). Data from the Boston Circulatory Arrest trial showed that at 8 years out (99), more patients in the circulatory arrest group had neurodevelopmental deficits than sufferers in the low-flow cardiopulmonary bypass group. This distinction was not present sixteen years out, however both teams of patients had neurodevelopmental deficits (100). Attention to perioperative modifiable components, similar to regional cerebral oxygen saturation may lead to higher neurodevelopmental outcomes. Using such a strategy, at 12 months, neurodevelopmental outcome was within the regular range (60) for patients having undergone the arterial swap operation. All adults with transposition of the nice arteries should be adopted a minimum of yearly by a cardiologist with expertise in grownup congenital coronary heart disease (101,102,103). Follow-up of particular person patients could must be more frequent and must be tailor-made in accordance with the clinical circumstances. Appropriate follow-up for all adults with transposition of the good arteries, no matter the type of restore ought to include noninvasive imaging, P. Freedom from readmission for cardiovascular reoperation calculated by the Kaplan�Meier method was 90% at 7 years. At least one coronary artery imaging modality (noninvasive or invasive) must be performed on all adults having undergone the arterial swap operation. Provocative noninvasive testing of the coronary arteries is really helpful each 3 to 5 years after an arterial switch operation. If positive, invasive testing with a cardiac catheterization should follow and if positive, interventional catheterization or surgical-based procedures should be pursued to treat necessary coronary artery obstructions (101,102,103). Prior to turning into pregnant, ladies of childbearing age ought to have an entire evaluation at a middle with adult congenital coronary heart disease expertise. While most girls who had atrial redirection procedures tolerate being pregnant properly, deterioration in functional class and systemic (right) systolic ventricular operate (without recovery in some), together with lifethreatening circumstances can happen (104,a hundred and five,106).
|
|